Reducing racial health disparities is a critical component of advancing health equity, and there's a role for all of us to play. Use our materials to learn about health disparities your employees may be facing, the impact it can have on your organization and what strategies you can use in your own workforce. You’ll get a clear sense of the challenges we're facing, the scale of health disparities related to key conditions and the costly impact it can have on your organization.
How are we addressing drivers of health?
Blue Cross and Blue Shield of North Carolina (Blue Cross NC) is leading the charge for health equity in our state – but it will take all of us to get there. Health care partners, employers, community organizations and other stakeholders all have to work together.
By taking this journey with us, you’ll learn why health equity and drivers of health are important. Find out how addressing health equity and drivers of health improves productivity, health outcomes of your employees and the financial impact on your business. We’ll also show how we can work together to advance health equity and reduce health care costs.
We are committed to improving individual and community outcomes with our powerful offerings:
- Tailored health plan solutions
- Strategies to address non-medical drivers of health
- Personalized programs to support those with chronic conditions
Do you know the cost of health disparities?
Every year, health disparities create huge economic losses for companies due to excess medical care costs and lower productivity.1
$93B
in excess medical care
$42B
in lost productivity
Health equity and your workforce
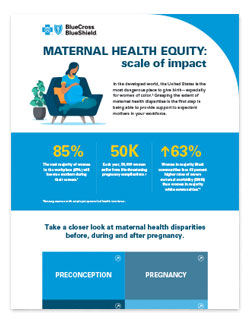
Addressing maternal health disparities
The United States is the most dangerous developed country in which to have a baby – especially for women of color. The risk for miscarriage, for example, is roughly 43% higher for black women compared to white women.2 That's just one of the many staggering maternal health disparities affecting the well-being of employees, which also leads to profit and productivity loss for employers. Learn more about these disparities, the implications on organizations and their workforces and how employers can help make pregnancy safer for all women. Our corresponding infographic lays out some of the staggering disparities mothers of color are facing before, during and after pregnancy, as well as how this impacts employers and organizations.
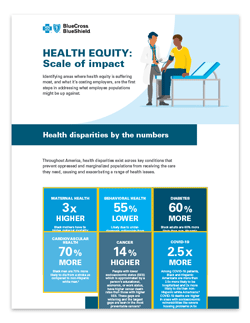
Addressing behavioral health disparities
Behavioral health conditions are on the rise across America, and disparities within behavioral health are having a serious impact across racial, socioeconomic and geographic groups. For example, estimates show that those of the lowest socioeconomic status are up to three times more likely to have a mental health condition.3 Learn more about these astounding disparities, their root causes, the cost implications on organizations and workforces and how employers can help forge a new path toward equitable behavioral health care for all. Our scale of impact infographic lays out many of the glaring disparities that exist across racial, socioeconomic and geographic groups, and the impact they are having on employers and organizations.
NC Health Equity Spotlight series
In conjunction with the Blue Cross and Blue Shield system’s National Health Equity Strategy, Blue Cross NC continues to drive smarter, better health care that's more inclusive and improves outcomes, both at the individual and community levels. View our Spotlight series to learn about our innovative initiatives around drivers of health, maternal health and behavioral health.
What are we doing to advance health equity?
Find out how we’re prioritizing strategies to address disparities that impact the health of our communities.
[MUSIC PLAYING]
[SCREEN TEXT] What's New at Blue?
Hi, I'm Beckie Brooks.
[SCREEN TEXT] BECKIE BROOKS
[SCREEN TEXT] Director, Drivers of Health Strategy
[SCREEN TEXT] Blue Cross and Blue Shield of North Carolina
I lead a team at Blue Cross North Carolina dedicated to developing strategies and actions that address non-medical factors impacting the health of our members. Here, and across the nation, the Blues aim to improve the health of all your employees and the communities where they live.
[SCREEN TEXT] Health disparities and drivers of health prevent many people from staying healthy and receiving the care they need.
Throughout the United States, health disparities and drivers of health prevent many people from staying healthy and receiving the care they need. We're talking about our neighbors, our friends and people in our communities.
[SCREEN TEXT] 1 MILLION PEOPLE are food insecure, Including 1 in 5 children
For instance, in North Carolina alone, one million people are food insecure, including one in five children.
This means they don't have consistent access to healthy food, which can lead to health issues later, like obesity, diabetes and hypertension.
[SCREEN TEXT] Inconsistent access to healthy food
Health issues:
• Obesity
• Diabetes
• Hypertension
Plus, a recent survey found that 40% of US households can't cover an unexpected $400 medical expense.
[SCREEN TEXT] Recent survey finds that: 40% of US households can't cover an unexpected $400 medical expense
[SCREEN TEXT] COVID-19 Pandemic
And on the heels of the COVID-19 pandemic, loneliness is also reaching epidemic proportions. Did you know that the physical impact of social isolation is equivalent to smoking 15 cigarettes a day? We know issues like these are important to you and your employees.
They can impact productivity, medical costs and the overall health and well-being of your workforce.
[SCREEN TEXT] Productivity, Medical Costs, Overall health and well-being of your workforce
That's what fuels our commitment to work with you on innovative ways to improve health equity and address drivers of health.
[SCREEN TEXT] We prioritize strategies to address disparities that impact the health of you and your employees.
At Blue Cross North Carolina, we prioritize strategies to address disparities that impact the health of you and your employees, including behavioral health, maternal health, and infant health.
[SCREEN TEXT] Behavioral Health, Maternal & Infant Health
We're also working with a number of organizations to explore ways to address non-medical drivers, like food insecurity, social isolation, lack of transportation and more.
[SCREEN TEXT] UNC HEALTH
We've joined forces with UNC Health in a groundbreaking clinical study to improve food security for impacted members who have hypertension. We are leading the charge with impactful initiatives and programs, but we can't do it alone.
We all need to work together to eliminate health disparities and positively move the needle on drivers of health in our communities. To learn more about how to address health equity in your workforce, visit BlueCrossNC.com/EmployerHealthEquity.
[SCREEN TEXT] BlueCrossNC.com/EmployerHealthEquity
[SCREEN TEXT] BlueCross BlueShield of North Carolina
[MUSIC PLAYING]
Addressing drivers of health
Explore how non-medical factors can impact the health and performance of your workforce. Blue Cross NC experts and others discussed drivers of health:
- The definition of drivers of health and the challenges created by the COVID-19 pandemic
- How non-medical factors impact your medical costs and workforce performance
- What can be done to educate, elevate and advocate for impacted populations
- Blue Cross NC’s drivers of health strategies to advance health equity, and how you can help
[Kim] Morning everyone. How is everyone doing today? Welcome to our addressing drivers of health session. We are so excited that all of you have chosen to join today. My name is Kimberly Evans and I will be the host for today's event.
I am a part of the drivers of health strategy team of Blue Cross NC and it is my pleasure to share with you all today.
[SCREEN TEXT] ADDRESSING DRIVERS OF HEALTH
[SCREEN TEXT] How non-medical factors impact the health and performance of your workforce.
[SCREEN TEXT] Webcast for HR professionals March 22, 2022
[SCREEN TEXT] Today’s Host Kim Evens, Senior Program Manager, Drivers of Health Strategy, Blue Cross NC
Just a bit of information to let you know that this is the first of a series of webcasts that we have planned for 2022, which is super exciting, and we want to talk about what's going on in healthcare. How do we provide innovation to make uh to deliver better quality, affordability and exceptional experience for all of those that are impacted by health, so we cannot wait to jump into this today.
We want this to be an interactive, um, webcast. We are going to have an understanding, we hope, by the time that we finish today we will all have a better understanding about the non-medical factors that impact the health and performance of the workforce and what are the things that should be considered when we are designing health plans? What are the differentiators that we need to improve employee retention, to help with productivity, and to mitigate, uh, at the end of the day medical expense.
And so, before we introduce our amazing panel for today, you guys are going to be awed, and just so, so, so, um, fortunate to hear from them.
[SCREEN TEXT] Housekeeping
• Your participation matters
• Submit questions via Q&Q box
• Eligible for SHRM PDC & NCDOI CE credits
• Take our Survey! HELLO FRESH $70.00 eGift card
A couple of things let's not forget that this is an accredited webcast. And that following this webcast you'll receive an email with a link for receiving your credits. And, we are asking everyone to please complete a survey after the webcast today. And if you do complete that survey, you will be entered for a chance to win a $70 hello fresh gift card and that is a great incentive to take just a few minutes to complete that survey, so we're asking everyone to please do that.
The other thing is, when we talk about how we want this to be interactive today, we are going to be asking poll questions we're asking everyone to please just tune in, make the most of these moments, get the most out of this information, respond to the poll questions so that we all can stay engaged together.
Last thing, we also have, uh, the chat set up for our Q&A. We won't stop throughout to make sure that we get you all of this important information, but we will at the end answer as many questions as possible and then we will make sure that we are reaching out, that we are sharing any information that comes up in the Q&A that we don't have the time to address, but we want to make the most of your time, so we'll sit them there. We'll filter through them. We'll look at common themes and then we'll come back to touch on for those for you all later. Cool? All right, let's get ready to get started because I am not the star of this show today.
[SCREEN TEXT] ADDRESSING DRIVERS OF HEALTH
[SCREEN TEXT] Today’s Presenters
[SCREEN TEXT] Heather Black, NC 211 State Director, United Way of NC
[SCREEN TEXT] Neal Curran, Director of Food Programs, Reinvestment Partners
[SCREEN TEXT] Dr. John Lumpkin, VP of Drivers of Health Strategy, Blue Cross NC
[SCREEN TEXT] Sandra McKinnon, Case Manager, Social Work, Blue Cross NC
We have an amazing panel and what we're going to do is allow them just a couple of moments, individually, to introduce themselves and to tell us a little bit about who they are, the work that they do, and we want to hear from them, what inspires them. So, we're going to go, you see the lineup, we’ll go just across of how the lineup is laid out here today and first we are going to start with Heather. Heather, please introduce yourself to our our visitors today and tell them a little bit about what you do and what inspires you to continue to do that.
[Heather] Thanks Kim, I am happy to do that. My name is Heather Black. I am the state director for NC211 with United Way of North Carolina and I'll just quickly share that 211 is a statewide information and referral service to connect people to health and human services through a free and confidential call by just dialing those three digits of 2-1-1.
So, we talk to a lot of North Carolinians, every day, who just need help accessing those very basic services and are often overwhelmed of how to navigate what can sometimes be a complex system to access those services. So, that's the role we play, is just to try to make that map of getting the services a little bit easier to navigate.
And what really inspires me and motivates me in my work is what we also learn about our callers and our clients through doing that work. We are very, um, capable of seeing trends in our communities very quickly through what we learn about our callers. We collect data and we look at it in aggregate form, not identifiable data, but sometimes we can very quickly, in a very real-time way, see something happening and escalate that up to our partners at our local United Ways across the state, our partners at community-based organizations, and in local and state government.
Um, just one quick example that we saw at the beginning of the COVID pandemic was a lot of North Carolinians that had been living in motels and hotels as their residency, and they were quickly in unstable economic situations due to the changes in our ability to go to work and were not able to maintain that housing. However, the eviction laws that were in place did not protect them as tenants. We had data very quickly to show that there was a large population of people who were going to become homeless if those eviction laws weren't expanded to identify them as tenants. So we were able to work with our, our partners at the attorney general's office and legal aid and get that expanded to protect those individuals. And that's what makes me excited about the work every one of those individual caller stories can come together and become something that we can really help advocate for a population. So that's a quick example. I have a lot more, but happy to be here. Thanks, Kim.
[Kim] Amazing! Thank you so much Heather and thank you for that example to help us to get focused on what we're going to be talking about today. Neil, will you introduce yourself?
[Neil] Sure. Hi, I'm Neil Curran, Director of Food Programs with Reinvestment Partners for a non-profit based in Durham, um, and we're honored and privileged to work with Blue Cross Blue Shield of North Carolina, among other agencies, other payers and providers to provide drivers of health programs, specifically in the areas of housing and food. As an agency, we run, uh, affordable housing units that like Heather was just kind of talking about, um, that's on the housing side. I'm on the food side and so we, um, I am very, again just so thankful to be able to work with Blue Cross and their drivers of health team, Becky Brooks, Kayla Epps, Lori Taylor, others who, um, have, led by Dr. Lumpkin, who and also working with, uh, case managers like Sandra who you both of whom you'll hear from in just a minute, but we distribute healthy food assistance benefits to um folks who are low income food insecure and struggling with a diet-related chronic illness.
We provide forty dollars per month for fruits and vegetables, distributed electronically, and so, uh, clients are able to get their benefits quickly. Um, it provides them with agency and choice to be able to pick out the foods that they like, within a subset category of healthy food, and people like it. So that's that's who I am and how I relate to this group.
[Kim] Thank you, Neil, and we cannot wait to hear more about the great work of Reinvestment Partners. Thank you so much.
Dr. Lumpkin.
[John] Thank you. I'm John Lumpkin. I'm vice president for drivers of health strategy at Blue Cross of North Carolina where we believe that we don't just believe it, it is actually our mission to improve the health and well-being of our customers our members and community. And part of that is addressing drivers of health. What really gets me engaged in this is, I'm by training an emergency physician. And I started out my career working in the emergency department. And it didn't take me too long to figure out that even if I gave the best care possible to each and every person who showed up at my door I could not fix the problems that resulted in them showing up in the first place. And so I began my journey saying that if I want to have an impact to really improve the health of people in my community, I had to do it by addressing those factors outside of my emergency department.
[Kim] Thank you so much John. We're ready to dig into your experience and your tenure as you have transitioned throughout your career, so looking forward to more discussion today about that expertise.
And then Sandra, will you please share with the audience who you are and what you do?
[Sandra] Yes, thanks Kim. Good morning, I'm Sandra McKinnon. For the last 16 years been part of a team of social workers at Blue Cross. We work one-on-one with our members. One of the common issues that we work with members on are financial needs, usually due to a temporary or permanent change in their health issues, which has resulted in time off work, loss of income, as well as increase in their medical expenses. So we work with them to try to connect them in with community resources like Heather was talking about, and Neil, as well as government resources, um, to try to assist them. As a social worker, one of the things that I'm inspired by lately is the movement within health care to recognize all the factors that play into a person's health and well-being not just the physical aspects of what being healthy means. Back to you, Kim.
[Kim] Thank you Sandra and we are so excited to hear more about your day-to-day experience dealing with the challenges that people encounter with regard to their health and all of the factors that impact that health.
[SCREEN TEXT] Learning Objectives
[SCREEN TEXT] 1. What are Drivers of Health
[SCREEN TEXT] 2. Scope of the problem and why employers should be concerned
[SCREEN TEXT] 3. What can be done to address non-medical factors
[SCREEN TEXT] 4. What are the results and what’s next
So what do we want to accomplish today? By the time we leave, we want to have a greater understanding of what we mean by drivers of health. We know there are a lot of different terms when we talk about drivers of health or the things that impact health that are non-medical so we want to get a better understanding about that. We also want to look at the scope of the problem. Why should employers be concerned? Why does it matter to all of us that we are addressing non-medical factors that impact health? What more can we do? As we learn today as we hear about some of the great work that's going on around drivers of health, what are some of the different areas that we can impact? Where can we make change? Where can we make things better? And then we want to hear some results, right? We don't want to just learn about them, hear about what's going on, but how are they helping. What is the impact? What are we seeing and we're going to share some of that with you all as well today. So, let's get our seat belts buckled let's get ready to jump in and learn more about drivers of health.
So let's start kind of level setting where we are with the poll question.
[SCREEN TEXT] POLL Which of these are considered drivers of health?
And the question is, which of these are considered drivers of health? Food security, healthy housing, social support, transportation or all of the above? Would everyone take a moment just to click and enter your answer there? Which of those are drivers of health? Yeah, and you guys are chiming in on the comments. I love it!
[SCREEN TEXT] Drivers of Health
Yes, yes you guys are starting out great this morning! Almost all of us entered all of the above. That is amazing, um, that is absolutely amazing, so yes all of those are considered non-medical factors that can impact um the health of an individual. Let's learn about why. Let's learn how.
Dr. Lumpkin, let's start with you. You can educate us I'm sure very well. Tell us what we're talking about when we use the term drivers of health. Who does it impact? What is the scope of this problem? Um, share your insights with us, there, please if you don't mind.
[John] Great, thank you Kim, and you know it's a pleasure and I'm thrilled that so many of you have chosen to uh listen in today. You know, I kind of am a numbers guy, so I'm just going to start out with numbers. Every year there's more than half a million minutes when you total up all the hours and days in each year. On average each person in this country spends just 60 of those half a million minutes in a clinical setting.
[SCREEN TEXT] Trends Signal a Critical Need for Change
[SCREEN TEXT] 60% of a person’s health outcomes are driven by social determinants of health1
[SCREEN TEXT] 50% of the U.S. workforce earns less than $35,0002
[SCREEN TEXT] 1 Joseph J. Fifer, “Social Determinants of Health: Pushing the Boundaries of Healthcare,” Healthcare Financial Management Association (HFMA), Oct. 22
[SCREEN TEXT] 2 Half of American Workers Made Less Than $35,000 in 2019, Report Shows. (2020, October 15). Newsweek. https://www.newsweek.com/half-american-workers-made-less-35000-2019-report-shows-1539503
So when you think about the factors and the things that influence the health of your employees, of people across the community, it's not going to be in those 60 minutes. It's what's happening in those half a million other minutes. Where people live, where they work and where they play. In fact, there have been some studies that have looked at it and found that anywhere from about 60 percent of the factors that influence health outcomes are these non-clinical drivers of health or social determinants of health that have an impact upon people's health. So what are they? And you saw that from the poll. I just have one complaint, Kim. They wouldn't let me vote!
I was originally born in Chicago. I'm used to voting two or three times, but uh so I'm going to tell you what I think they are because, in fact, you all got the answer so well. They relate to housing. You know we think about how much medication we give people to treat their asthma and unless we address those triggers that are in their home their asthma is not going to get better. One of the most costly medical conditions that frequently, and particularly for seniors and those older that lead ultimately to death, are falls in the home and simple repairs around the home removing tripping hazards can reduce the instance in all of these, falls or asthma, are high cost procedures that lead to increased costs for everyone. They involve transportation. It's easy when I was working in the emergency department to write a prescription and say, ‘get your medication.’ But if I wasn't thinking about how does that person get from their home to the pharmacy that prescription would go unfilled. Social isolation, the fact that people sometimes are isolated from their neighbors, is strongly associated with significantly higher costs. And how many times does a physician say to a person with diabetes, ‘You need to eat good foods and you need to exercise.’ And that person leaves saying there's not a grocery store in my community.’ or ‘I'm kind of afraid of going out on the street at night and walking.’ So if those conditions are addressed we can't begin to do the kinds of things that help people to be healthy.
And then the big one, is food. Fifty percent of the US workforce earns less than thirty five thousand dollars. And that's important because when we think about food and food insecurity, in other words, someone who has not had consistent access to food over a period of time, we think about people who are in poverty. Yet, the data has shown that half of people who are earning thirty thousand dollars or less are food insecure. And some of those who earn more because each has a family situation. It could be with housing rates going so high here in North Carolina. It could be transportation because the car breaks down and all of a sudden towards the end of the month they don't have enough money to purchase their food.
[SCREEN TEXT] North Carolina ranks the 10th HUNGRIEST STATE1
[SCREEN TEXT] ACROSS NORTH CAROLINA more than 600,000 ARE STRUGGLING TO PUT FOOD ON THE TABLE1
[SCREEN TEXT] Berkowitz, S. A. (2019) State-Level and County-Level Estimates of Health Cre Costs Associated with Food Insecurity.
And it's strange because, you know, North Carolina is the eighth largest agricultural producing country or state in our country, yet we're also the state with the 10th highest rate of food insecurity. These are the factors that have an influence upon the health, the outcomes, and importantly the health care costs. And these are the same factors that influence whether or not that employee shows up to work, ready to give them their all or if they show up because they're sick, not able to work, or they're thinking about what their family is going to have for dinner because they don't have enough money. All of those take them away from being the most productive individual that they can't be. This is why we begin to talk about and focus on these drivers of health. Kim.
[Kim] Thank you Dr. Lumpkin, um, really appreciate that educational moment for all of us to learn more about the impacts of drivers of health. And Heather, when I think about the work that you do with United Way 2-1-1, you guys are the boots on the ground that are talking to folks every day. And you shared a little bit in the beginning, but can you tell us a little bit more about what you hear the most, what are the most common requests or calls that you all receive at united way 2-1-1?
[Heather] Yeah, so much of what Dr. Lumpkin just said resonated with me. You probably saw me nodding my head along, um, because it is, it's reflective in our call data that you see here.
[SCREEN TEXT] 2021 Top Needs for North Carolina
• Housing & Shelter 98,478
• Utilities 40,963
• Employment, Income & Family Supports 16,909
• Healthcare & COVID-19 9,218
• Government & Legal 6,333
• CALLS 160,937
• NEEDS MET 194,100
So these are our top caller needs from 2021, and you can see it aligns almost exactly with what Dr. Lumpkin just described, so housing and utilities. If you can't, if you don't have stable housing, if you don't know that when you go home tonight you're going to feel safe and cozy and comfortable, and that the lights are going to be on, that the heat is going to be able to be on in the winter, or the fan can blow in the summer, um, and again if you have a chronic health condition those kinds of things are not just a comfort, or to make you feel good, they can sometimes be health essential, um, if you can't keep those things going then that can be a big factor in your overall health. Again, if you can't put food on the table and you're worried about that or you're worried about your child being at school and being hungry and not being able to be productive as a student those things all impact your overall health.
And I think the other thing that really resonates for me, when I look at these numbers, because these are all things that have always been top needs, you don't see food insecurity here because we did find over the last two years during COVID, interestingly, that food dropped out of our top caller need. And I think that's because there was such a response at the community level, and also additional benefits through SNAP and EBT programs to make sure that people did have food.
I don't think that means that there's not still a need. I think it means that those needs are being met in different ways. Um, you know we always hear, especially I know I always heard growing up you know we're all one maybe two bad things away from you know paycheck to paycheck type thing. And I think COVID really was that level setter for a lot of families, that one emergency. You know it wasn't a car breaking down it was a global pandemic and I think that's what we're seeing a lot of folks who need who never needed this kind of help. They were able to make it. They were barely making it, but they were able to make it. And now, there are a lot more individuals who are in situations where they are relying on social services. They are relying on government assistance, but they are employed. These are people who are employed. They were employed before the pandemic. They are they were employed through the pandemic, to the level they could be, based on what our, you know, state circumstances were and whether they were, you know, in jobs that you could continue to do during the pandemic. They now are either underemployed or perhaps, um, as Dr. Lumpkin alluded to, the income they're making is just not enough. Um, you know, I was just talking to my mother this weekend about the cost of groceries increasing and how our families are able to manage it but there's probably a lot of families that aren't. So you know we grow ripe and grumble about it but there are families who really that dollar increase in a box of cereal is a make or break it. And I think we have to be thoughtful about that and understand what that really means for some families. The choices they're having to make and then that leads to second- and third-level needs that are not even getting addressed because there's so much focus on these first level very basic needs.
[Kim] Thank you Heather and I love that you hit on that word that stood out to me, their choices. The choices that people are having to make are now often different choices than they've had to make before.
And Sandra, I'm sure you hear this every day when you're on the phone talking with folks and they're making hard choices. They're having to face decisions that they haven't before. You've been doing this for a while and you know we are now beginning to talk about drivers of health a lot more, social determinants of health, and, um, but you've been hearing this stuff for a long time. How does this impact people that you talk to every day?
[Sandra] Right, yeah, and to echo some of what Heather was saying, I mean the pandemic changed a lot of things for people, um, certainly pre- pre-pandemic, the sorts of issues, um, in terms of financial strain that I was helping members with was usually due to medical expenses. Since the pandemic hit, now those needs have switched over to you know paying rent, utilities, uh, groceries. And when I'm working with families that are under financial strain and food insecurity, I mean they are making those tough decisions.
You know, I think any of us were under financial strain we start to look at how can we allocate our resources. You know, where do we need to put the money that we have and what are things, you know, what are expenses that we can cut or that we can, bills that we can push off until next month? And, unfortunately, with families some of these you know the byproduct of some of these decisions they're making is impacting their health in a negative way. Uh, you know, people are telling me they're not filling their prescriptions or they're not taking them as prescribed. They're not going to follow up medical appointments because of the co-pays or having follow-up medical tests. And this is affecting their ability to manage their health. In some cases, it led to ER visits, time off work.
You know, another thing that happens when you're worried about having enough money for groceries, it affects the types of foods that you purchase. And healthy foods tends to be more expensive food, so when you're choosing less healthy options based on cost and if you have a medical condition that's affected by your diet choices, like high blood pressure or diabetes, then that you know that starts to affect your ability to manage these, you know, conditions effectively.
Um, so there's a lot of things that start to impact a person on a you know a daily basis. They're also looking at the the mental health effects, too, the stress of worrying about having your money last to the end of the month. Um, you know, people share with me, you know, they're not sleeping well. This the stress and anxiety they're having trouble concentrating at work. They're concerned about their children concentrating well at school. So, um, there's a lot of things that that start to factor in.
[Heather] The other thing I would add to that, and you probably have heard this Sandra, is dental care, eye care, things that are, you know, not typically covered by your primary insurance that can lead to long-term health effects if they're not treated. Um, that often that's something that really quickly falls to the wayside for a family facing financial challenges.
[Sandra] Absolutely, absolutely. And to echo you also Heather that the pandemic, there was a lot of people that were in need of accessing resources that had never had had to access resources before. You know people would often tell me, you know, I've always worked. You know? I've always been able to pay my bills, care for my family, and then the pandemic happened. And if you didn't have a you know um a safety net of savings you know there wasn't time to put one together. You know jobs were furloughed people were sent home. So there was you know a lot of uh scrambling to educate people of what was available. What they could tap into and and how to do so. Um you know and also making sure that these services um people are accessing them in a way that feels respectful to them, as well.
Yeah and it also contributes as you've alluded to to the mental health impact because then there's anxiety and depression and and shame of having to ask for help when you've never needed it before. And it's, you know, I think those are all normal human emotions in those scenarios. Obviously the folks that work in these fields our team at 211 and I know Sandra's team we're reassuring them that it's okay to ask for help. But there's still just that human pride of of not wanting to ask for help and then that has just that other layer of impact to an individual. So it's it's definitely a snowball effect.
[Sandra] Yeah, absolutely. Stigma can really be a big obstacle in being able to access services and, yeah, I mean people were sort of literally giving themselves permission to access services and ask for help. So yeah, yeah.
[Kim] Absolutely. Thank you all for that valuable information. Talking about because oftentimes when we think about drivers of health or things that impact health. We think about those direct things but there are so many indirect things that impact health. There's so many domino effects that kind of stack on and stack on when we talk about drivers of health. So thank you all for bringing that point to the light.
Believe it or not we are halfway through and so let's do a little bit of a pop quiz with another poll question to make sure that we were all listening to Dr. Lumpkin.
[SCREEN TEXT] POLL What percentage of a person's health outcomes are impacted by non-medical factors?
Would you all take a chance to take a moment to fill out the poll please? Just to keep us all going, keep us all revved up. Awesome, and we'll get some results coming in from that.
[SCREEN TEXT] Approach and Programs
Let's see, we got 60%, 70%, 50% all pretty close. Those are good guesses. So when we talk about those health, um, outcomes being impacted it is 60. Sixty percent of an individual's health outcomes are driven by non-medical factors drivers of health that impact the actual physical health. And as Sandra and Heather talked about there are so many facets to health, not just that physical health but emotional well-being mental health all of those things that are impacted, which is why it makes sense for us as employers to make sure that we are thinking about drivers of health when we think about those medical costs but also thinking about presenteeism in the workplace, thinking about productivity in the workplace, the way that workers feel, um, when they are seeking assistance in the workplace makes this very very important.
So, now my daddy always told me don't tell me the problem unless you come with a solution. So we come today to talk about what are some of the things that we can do about it? What are some of the things that are actually in play? And we want to pivot to Neil to share some of the amazing work that they are doing at Reinvestment Partners. Neil will you please tell us a little bit about what we're doing about drivers of health? What are some of the programs that Reinvestment Partners has implemented to help folks address some of these needs that we've talked about?
[Neil] Sure, yeah, thank you. Um, so again, I work for Reinvestment Partners and we're a non-profit in Durham, a human human service organization. We provide services for low-income individuals that are feeling the squeeze on all sides as was kind of discussed prior in the prior section. Housing, consumer finance, transportation, these are the areas in which our organization works. I work in the food side. On the food side, we run a what we call a produce prescription program. Essentially, it's money to individuals who qualify for the program to purchase fruits and vegetables with no added salt, sugar or fat. And we were again fortunate and thankful to work with Blue Cross to distribute these benefits to over,, uh 5,400 of their members who qualified on their ACA qualified plan. We used we partnered to perform outreach. The eligible participants were then able to enroll themselves into the program. We received those participants’ information and were able to distribute the benefits that were loaded onto a Food Lion customer loyalty card. The MVP card maybe some of you have some of them and shop at Food Lion. The funds are loaded electronically. The clients by simply swiping the card at checkout can purchase any eligible item, which again was fresh, canned or frozen fruits and vegetables with no added salt, sugar or fat. We saw a relatively high uptake on the outreach side and on the redemption side we saw about 85% utilization, which checks out with our other programs. So it's a fairly simple program. We pride ourselves on quality customer service, which is something we align with Blue Cross on and also efficiency or another area we align where we think that folks they know what they are in need an urgent need. They know how to use the benefit, we just need to get it to them. Um, I’m not a data person. I work for a non-profit, so I’m much more interested in stories. And I’d like to share just a few stories from participants that we served with the program to hear how it impacted them. I think you'll find it impactful, as well.
‘This program helped feed, this program fed me during my pregnancy, and my young child. There were nights that if we didn't have those fruits and vegetables, we wouldn't have anything to eat.’
Here's another one, ‘It really helped. Food prices have gone up through the roof. It's hard to buy food on a budget. With the extra help with fruits and vegetables, it was a lot easier. Fruits and vegetables are usually what I have to go without.’
Last one, ‘It was a tremendous help for me because it helped me to buy other things with the little money I had coming in and still be able to provide my children with the healthy items they need.’
Um, I'll do one more just because I think it's better to hear stories than to hear me talk. Um, last one, ‘It was very helpful because I'm a diabetic and got real sick in 2020 and the fruit and vegetables are the best diet for my condition. Eating the fresh fresh fruits and vegetables really helps me keep my sugar under control. Without this program I don't eat as much fruits and vegetables and I do see my sugar rising a little. I really appreciate it. Thanks everyone involved.’
Um, so those are just a few of the stories. We have countless more and I hope maybe you're hearing some themes coming through in those those anecdotes from the prior discussion of how people have to make trade-offs. People have to make choices they have their their working folks. Uh and they're they're kind of put in these impossible situations where it's do they choose the healthy items that they know they should eat because we all know we should eat more, you know, an apple a day keeps the doctor away or do they need to get the most bang for their buck with their limited dollars. Um, and and, you know, it's it's complicated right? We / I know this. People like Dr. Lumpkin said at the top, North Carolina is an agricultural state. There's plenty of food to go around. So the question is less about is the food there. It's how do we maintain people's access to these uh products, these the healthy foods, over time so that it's stable. And they can rely on it make their own choices and have some agency and dignity in how they receive, um, the benefits and how they acquire the healthy food. These are important questions and we're really glad that um Blue Cross is um out in front and we're glad to be there with them.
[Kim] Neil we love hearing about that food prescription program absolutely amazing and those stories are amazing. Are there any other reinvestment partners programs that you'd like to share today or provide any insight about any of the other services.
[Neil] Sure, I'll just quickly mention a few the other ones. I’m less involved with those, but we do run a volunteer income tax assistance clinic. Um, the state we have about through our subsidiary partner agencies we serve about 30,000 people a year so they, um, for low-income folks to get their taxes done for free, which as you know that's a so many people lose the money that they the government owes them simply because they don't file their taxes. So that's one example. Another is our we do some housing work. One example is a program for children with asthma. So as you know emergency department visits are really expensive and there's a lot of triggers in the home that cause uh uh people, children especially, to have asthmatic um episodes and they wind up in the emergency department. Well, there's there's a suite of products that we provide through our what we call Breathe Easy at Home Kit. Things like, um, pillowcase um sorry I’m kind of reaching here, but we have a Hepa filter vacuums, dehumidifiers, uh antimicrobial sheets, things like this, you know, of course the best thing would be to get those kids into a home that doesn't have the asthmatic triggers like mold, pests um water issues etc. but short of that because that's that's uh you're talking about landlords and you know property issues, anyways these are that's another example.
[Kim] No that's helpful Neil thank you so much um because we're still talking about non-medical factors that impact health of folks. And so he shared about the um eat well benefit, the food prescription program with reinvestment partners, but Dr. Lumpkin can you share with us a few of the other programs that Blue Cross NC is offering to address non-medical factors that impact health?
[John] Great, thanks Kim. It's, you know, it's really an important part a new development for us at Blue Cross and we take the approach that just like you said Kim, what your pappy said, ‘don't come to me with problems, come to me with solutions’ and the problem is is that the medical literature has all sorts of articles of how these non-clinical drivers of health impact health costs, lead to higher costs. We want to get to the bottom of it. What actually helps reduce those costs, lead to better outcomes and lead to more satisfaction of our members.
Now, Neil talked about the programs being well received and he also talked about them being efficient. What we also look to do is to make sure that they are effective. And so in addition to working with Reinvestment Partners on the on the food prescription program that we call Eat Well. We also have a program that we are testing related to food delivery. And in this particular program, we work with a company that delivers a shelf stable, in other words a box of food that people can use to produce and make healthy foods within their home, and we link that up with food and nutrition coaching and this can make a dramatic difference. And we've just heard stories, one that just sticks with me, uh, is about a man who said he used to share his insulin with his brother and then after he was able to get the food box he could buy his own insulin as well as eat healthy food.
We also have another program that we work that we're assessing with a company called Papa and they have associates, Papa Pals they call them, who work with people who may have, uh, maybe shut in because they have difficulty walking, difficulty hearing, poor eyesight or a severe chronic illness and these Pals will talk with these individuals on a regular basis, help drive them to the doctor, drive them to the food store or to the pharmacy. And then finally, we're looking at trying to really build the evidence base in what is the really the the gold standard in clinical and medical work. And trying to convince others to do it, which are randomized controlled trials. And we're doing this in partnership with the University of North Carolina at Chapel Hill and their health alliance. And that is comparing two different approaches the food prescription one you heard Neil talk about, as well as a food delivery approach, and see which one gets the best results as well as tying it into coaching. And then here's the extra part, which we think we're the only ones who are looking at it. What is the right duration for these interventions? Medicare policy says that for people who are on Medicare Advantage that the benefit for food can be two to four weeks after hospitalization. There's nothing magical about that time frame if you have somebody who has diabetes and I as a physician are prescribing insulin and they come back to me after six months and say my my diabetes is under control, I don't take them off the insulin yet that's the way we treat many of these non-clinical drivers of health implementations. And so we're doing this randomized control trial to have some of the people on the trial for six months and some for 12 months to create the evidence that can influence not only what we do at Blue Cross, but policy in North Carolina and across the nation. So that everyone can have access to the programs that will help keep them healthy and when they're ill help them get healthy again. Kim.
[Kim] Thank you Dr. Lumpkin. and Neil and remembering that these interventions these programs that we're talking about are helping working people. These are helping people who are working every day, but having to make those tough choices. So speaking of tough. Sandra I’m not putting you on the spot, but I’m gonna put you on the spot! You've heard from Neil, you've heard from Dr. Lumpkin, as you talk to people every day what are your thoughts around these interventions in these programs? Do you think these will help the people that you talk to on a daily basis?
[Sandra] Yeah, absolutely, being able to offer these programs to our members over the last year or so has made a huge impact. As Dr. Lumpkin said instance where people are sharing their medications um so being able to have access to that forty dollars per month through Eat Well allowed that gentleman to be able to shift his money from the groceries in order to be able to start purchasing purchasing his own insulin. Um, you know that another program that we've been working on at Blue Cross is to ensure that our members who have who are eligible for SNAP, which is the government issued food benefits are aware of the program and how to access it. Um, for example, I’m speaking with a woman recently she was employed, married, mid-40s, her husband had a recent surgery so he was out of work for a while and they had incurred some higher medical expenses. In my conversation with her, she said that they were having difficulty, you know, making their money, uh, stretch every month. I felt that she might be eligible for the SNAP program and we discussed it. She was aware of the program but she hadn't applied. It's a common misconception that if you're employed you're not eligible for SNAP benefits. And we had here at Blue Cross partnered with a company that's helping our members apply. It can be a rather cumbersome process multi-page and it entails either doing it online or going to the local Department of Social Services for this woman that I was working with um she didn't have reliable internet access and it would mean her taking time off work to go down Department of Social Services to see if she would be eligible. And she wasn't very motivated to do so as she felt that she probably wouldn't you know be eligible. She didn't want to take time off work and incur even more financial strain. Um so being able to transfer over to a company that we were using they were able to assess her for SNAP benefits, take the application information and submit it electronically. Um was you know a huge help for her she was able to do that over the course of her lunch hour and not have to take you know time off work to access resources. And in my follow-up call with her, she had been approved for SNAP benefits and that was really you know helping out until her husband was able to, um, to get back to work because often food insecurity is a situational, um, event or a seasonal event and sometimes you know people just need some some temporary help. Um, you know in order to to get back to where they were. So definitely every day I’m seeing the positive impacts of being able to offer programs and not only offer programs but be able to have an easy way to access these resources. It's important as well.
[Kim] Thank you, thank you for, um, verifying that for us Sandra that these programs are on the right track. And I know Neil you said hey I’m not a data guy. Dr. lumpkin you said you are, so I wanted to make sure to follow up because I know folks that are listening employers that are listening like hey this is all well and good it makes perfect sense.
[SCREEN TEXT] Impacting more than 10,000 MEMBERS Addressing non-medical drivers of health1
1 Blue Cross NC Drivers of Health Strategy Program – Q3 2021 Performance Report
2 1M: https://mediacenter.bcbsnc.com/news/blue-cross-nc-announces-new-and-innovative-programs-to-boost-heath-across-north-carolina
It's intuitive people need food. People need housing. All of the things, but what results are you seeing? What's what's the bottom line? What are we seeing when we are making this investment into drivers of health? And so Neil you can just show up share a few things that you guys have seen as you've been able to analyze some of your programs. In the end Dr. Lumpkin if you follow up with some of the things that we have seen at Blue Cross NC.
[SCREEN TEXT] Effectiveness and What’s Next
[Neil] Sure, um, so on the data side, I’ll share two data points one is 95 percent that's our net promoter score for the Eat Well program, which according to being the main company that came up with the net promoter score metric that counts as world class anything over 80 / 85 percent is uh doing doing is about as good as you can. So 95 percent, we're really proud of that number actually. Um it just means that people really like it. They're really likely to recommend it to family and friends, which if they're likely to recommend the program they're likely to recommend the plan as well.
Um the other data point I would uh offer is is uh uh 2X uh our program the in a study per um that we participated in with Dr. Seth Berkowitz. Um and published a paper in JAMA, uh, open we are the findings from that study found that participants on average almost doubled their um fruit and vegetable consumption. That's pretty big. People were only eating, purchasing, consuming about 35 dollars worth of produce per month. And so we added another forty dollars per month to the budget and they doubled it, which equates to about an additional serving of fruit and vegetables per day per person in the household. So that's while that that's only one serving doesn't seem like a lot but if that is doubling your amount that you're eating and if your goal is to get to five servings per day, which is what the USDA recommends it's a pretty sub uh significant increase. So what we're excited about in the future is to see if giving people more money actually gets us closer to that five servings per day number. Um and that's that's kind of uh Dr. Lumpkin asked this question about dose and duration. Those are questions that we can
look further into in the future. Um but yeah, so it's it is an effective program people do use it.
[Kim] Thank you. Dr. Lumpkin?
[John] Thank you Neil for for sharing those those numbers and um, you know, I’m a little bit surprised sometimes that we actually get to the point of saying, ‘How effective are these programs and why aren't we doing it?’ Over 2,000 years ago, Hippocrates, the epitome of what people think about as a physician, but 2,600 years ago he said, ‘If you want to know about the health of the people, look at the air that they breathe, the water that they drink and their diets.’ So when we implement these programs, we also look at their effectiveness. Not only just the incredible stories of how it affects individuals but looking at them overall, and let me tell you just about the one program the Food Delivery Program where we have completed this the the initial study and we have the beginnings of the numbers back. Individuals who are part of this program both ACA and some commercial members had diabetes and they had a reduction in their A1C. This is the number that doctors use to tell how well their diabetes is controlled and when those numbers go down that means people are in better control and healthier. And what we expect to have within the next month or two is the numbers about medical costs. Now this was a trial for six months and sometimes those cost savings don't show up right away but what we believe we can demonstrate is that these kinds of interventions not only are well received, and they have clinical impact, but overall they will save resources that can then be used in the health care system to treat others. These programs have impact on people's lives and impact upon the effectiveness of the health care system itself.
[Kim] Awesome, thank you so much. And then one follow-up question. As we've talked about this today, talked about why it's important for the workforce that's what we want to make sure that we're dealing with today. While we're understanding that drivers of health impacts people all the time and as Heather said, you know people are incurring things that they never have before if you had, you know, the ability Heather to impact employer decisions to impact employer benefits. Based on what you hear every single day, what would you say that employers can do to help lead the way?
[Heather] That's a great question. So I think we've talked about it. We see it every day on the news about the disparity between the cost of living and the wages that people are making right now, and I’m not going to get on a soapbox about wages, but I think what employers can be doing is thinking about how they can make investments into the communities where their employees live and strive to be healthy. Neil and Sandra and I have all talked today about the reliance of people on social services, health and human services, in the community. Dr. Lumpkin talked about that as well and how that impacts overall health of our communities. So I would encourage employers to be looking for opportunities to make those investments. Neil’s program, the program that Sandra’s been talking about, that she's sending employees to, or individuals to, those programs are only there when investments are made to ensure that we're there. We are a safety net um to to catch right to catch folks and we we ramped up and and we were there during the COVID pandemic. um I think we've all seen now that that life before the pandemic we I don't think we're going to go back to that. I think that this level of urgency this level of need will continue at least for the foreseeable future and that is where then we're going to need more investment into our network of community-based organizations, non-profits to make sure that we have um additional help to fill those gaps. We're doing a unique thing with Blue Cross to support their employees. I’m utilizing 2-1-1 and having a special navigator there to make sure that they have access to as many resources as possible. So I would just say, you know, I know employers do already but be thinking of how you can make those dollars investments into the communities where your employees live.
[Kim] Absolutely, and you touched on one thing we didn't mention today, Heather, that is our partnership with United Way 211 the Blue Assist Navigator Program that is designed specifically for Bue Cross NC employees at the moment to be able to tap into and have knowledge around all of their benefits as well as the wealth of resources that are available through 2-1-1. So that is a program in addition at Blue Cross NC to help make sure that we are addressing all of the factors that could impact our employees. [Heather] And I think that's a really unique week that was just that's a unique way that Blue Cross really saw a potential gap and stepped up and said hey maybe this is how we can better support our employees during these times. And I think that's a really unique model that we've come up with and I’m excited as you know. And it's new, so we're going to see where it goes kind of like Dr. Lumpkin said, we're going to watch it and study it and get the data and get the stories and hope that that model proves to be what we think it has the potential to be.
[Kim] Absolutely, and as we you've heard today we've had a lot of focus on food but remember from our poll there are a lot of things that can impact health and as we continue this work continue to drive forward then we'll be looking at more of those factors and how we can impact um those as well.
So let's talk about as we come to our last four minutes get ready to close out today. Um what are our um key takeaways?
[SCREEN TEXT] Key Takeaways
1. A new approach to health care is critical for employees’ total health and wellbeing
2. Focusing on Drivers of Health as part of your health benefits is critical to the performance of your workforce
3. Awareness is growing, more programs are available, and new partnerships are forming to address these issues head on
Hold on I think we got one last question. Let's get this in here to make sure we address. Um how do we create awareness about these programs and resources that are available um to the community? And I think um Heather you'd be a great person to weigh in there, and then Sandra, how do we educate other employers about these programs, which is what we're trying to do today but how do we share this information because we do want to be a leader in thought leadership around drivers of health. How do we how do we create more awareness? And anyone who wants to try me and feel free but Heather I think you'd be great.
[Heather] Yeah I’m happy to kick it off. So I think you do have already great robust programs happening. So often um in communities United Ways are the the collaborators. We bring a lot of organizations together to collaborate so I would always encourage folks to reach out to their United Way. Um we have you always have opportunities to get involved on boards um get your feet get your feet a little dirty get your hands a little dirty. Get out there. Find out what's happening and be that voice within your organization. I think that's the best way and I would always say don't reinvent the wheel. Go see if the wheel's already been created in your community and how you can support it. I think all too often um we learn of a problem and we think we'll all go solve it but maybe someone already has and they just need more energy behind it. So uh that would be my encouragement it was to get out there and find out what's happening.
Awesome. Any other ways Sandra? That you suggest to create awareness?
[Sandra] Well I think creating awareness um you know we need to partner with all sorts of different you know resources and providers so that people can be aware of what resources are out there whether that's through um medical clinic, whether that's um through their employer, it's a way to um also wellness platforms or a way for a person to self-refer. Um to get help as well and it's a lot of sort of you know building trust and getting back again to making sure the resources are there and that they're being provided in a way that is respectful for you know for people's needs. Were you chiming in Dr. Lumpkin?
[John] I was I just wanted to add one other piece at Blue Cross we are a North Carolina insurance company. We're based this is where our focus is. We're committed to our members and their communities and so as we're addressing and developing evidence this is not evidence we're going to keep under a a basket but we're going to publish the evidence so it's available for employers to think about as they're designing their benefit package. But we're also going to make it available to other insurance and and the feel that whole we don't think that we compete on the issue of helping people get healthier or addressing these non-clinical drivers of health. Rather, we think that our job job is to think about not only our current members but people who will be our members next year or the year after and we think about everyone in North Carolina and so our goal will be to try to make sure everyone is aware of how important these issues are as well as the fact that there are things that we can do so that everyone has a fair opportunity to be as healthy as possible.
[Kim] Great wrap up Dr. Lumpkin. Thank you to all of our panelists. You guys have been amazing as well as educational informative today. We're looking to make sure that we have learned today that addressing drivers of health is key. It is critical to addressing the total health and well-being of our workforce making sure that we are keeping the things that we have learned today top of mind and that we are um reaching out to our Blue Cross NC representatives. If you want to learn more about these solutions or how to deliver more quality lower cost and better overall experiences for employees and families then please contact us and we will be happy to share that information.
[SCREEN TEXT] ADDRESSING DRIVERS OF HEALTH
[SCREEN TEXT] How non-medical factors impact the health and performance of your wordforce bluecrossnc.com/addressing Drivers
[SCREEN TEXT] Take our survey for a chance to win! HELLO FRESH $70.00 eGift card
Thank you so much don't forget to take your survey, get entered to win that $70 gift card and then you'll receive a link to get your credit for today's course. Thank you everyone.
Advancing health equity together
Discover where health disparities are affecting employees, challenges the pandemic has created and how advancing change will take all of us. Experts from Blue Cross and Blue Shield discussed the greatest health equity challenges and opportunities:
- The scale of health disparities and their impact on employee populations, and how that’s costing employers
- What health plans can do to advance health equity, and how the Blue Cross and Blue Shield system’s National Health Equity Strategy is confronting the issue
- How health plan partners, employers and other stakeholders can work together to help change the tide, highlighting specific strategies to focus on
Introduction
[Albert Chu] Hello everyone. Welcome and thank you for tuning in today. I’m albert Chu
executive director of health analytics at Blue Cross Blue Shield association. I’ll be moderating today's discussion.
I’d also like to welcome my fellow panelists whom uh I’ll introduce in just a moment and thank them in advance for joining in this critical discussion about the health equity crisis in America and its impact on the workplace and workforces across the country.
Advancing health equity will take all of us. The pandemic a wide range of cultural shifts and the transition to the next normal that we're all living through right now are certainly affecting the issue to say the least but what's really important is moving from talk to action.
Agenda
In our discussion today we'll highlight perspectives about what stakeholders and healthcare must do. We'll provide strategies employers can take and are taking to make an impact and we'll show how we can move beyond just our own individual roles to the level of coordination and collaboration needed to support amplify and take action on what we can do together and differently.
We just released the first in a health equity series of mini e magazines which you can download a copy of the mini e magazine and other helpful resources and the resources to download section of this webinar. We'll also have time for Q&A at the end of our discussion today so if you have any questions along the way please put them into the chat function and we'll cover what we can in that portion of the program later on but without further ado it's my great pleasure to introduce my partners in today's discussion.
First Dr Adam Myers is senior vice president and chief clinical transformation officer for the Blue Cross Blue Shield Association. Dr Meyers drives clinical transformation across the Blue Cross Blue Shield System through national networks quality initiatives and policy and advocacy positions. In his role he collaborates with the chief medical officers across all of our 35 Blue Cross Blue Shield companies and leads the office of clinical affairs and the Blue Cross Blue Shield Institute. A long-time advocate for community health and health equity Dr Meyers helped set the vision for the Blues efforts to create a more equitable health care system.
Next we also have Bridget Hurd who is vice president of inclusion and diversity and chief diversity officer at Blue Cross Blue Shield of Michigan. She also leads the office of health and health disparities focused on achieving health equity in care delivery and access. And she manages the diversity leadership council driving cultural competency learning opportunities for employees.
In 2020, Bridgette was appointed by Governor Gretchen Whitmer to the Michigan Coronavirus task force on racial disparities and was given the Dented Quest Healthcare Heroes Award for addressing health equity in the age of COVID-19.
And finally, Amanda Smith chief engagement officer at Morgan Lewis and Bacchus, one of the 10 largest law firms around the globe with thousands of people in offices worldwide. As part of her role she's been instrumental in developing and leading the organization's diversity equity and inclusion and well-being programs. Some of you may have seen Amanda join us in a previous webinar we hosted on behavioral health and its impact on workforces. And so it goes without saying that we're thrilled to have her back.
Adam, Bridget, Amanda, good afternoon to you and good to have you. Thanks for joining and letting your part of today's panel discussion health equity.
Now before we dive in for all of us and for those in the those of you in the audience I’d like to provide some quick grounding to help frame today's discussion.
[SCREEN TEXT] Slide 1 Defining health equity
[SCREEN TEXT] Health Equity is the absence of unfair, avoidable or remediable differences in health among population groups defined socially, economically, demographically or geographically or by other dimensions of inequality. (World Health Organization)
Defining Health Equity
To start off health equity is a term that's being used more frequently and is becoming more common in our broader social and professional conversations and it can certainly mean different things to different people so we want to be clear about how we're defining health equity for the purposes of this this discussion today. This is uh the World Health Organization's definition and the one we've committed to in our health equity efforts.
Health equity is the absence of unfair avoidable or remediable differences in health among population groups defined socially economically demographically or geographically or by other dimensions of inequality. We also refer to gaps in health equity as health disparities. We'll talk about many of those disparities today highlighting the scale of their impact on people's health and well-being as well as on organizations.
[SCREEN TEXT] Slide 2 Health disparities by the numbers, across key conditions employees are facing
So let's go ahead and jump in and start.
Health Disparities Related to Key Conditions
With a look at health disparities related to key conditions employees are facing and here you can see right off the bat our research here shows that regarding maternal health maternal mortality is three times higher and morbidity two times higher for black mothers than for white mothers. We look at behavioral health and this is likely due to under diagnosis from what we've seen millennials from majority black and Hispanic communities have lower diagnosis rates than depression 31 and 55 percent lower respectively when compared to white communities. Studies show black adults are 60 percent more likely than non-Hispanic white adults to be diagnosed with diabetes and in terms of cardiovascular health our evidence highlights that black men are 70 percent more likely to die from stroke as compared to non-Hispanic white men.
Of course it goes without saying that we should also acknowledge COVID-19. Given what continues to be top of mind right now for all of us and the part that is played in exacerbating disparities across all of these conditions and others as well.
So I’d love to open things up here for a moment for some initial perspective uh from our panelists. Uh Bridget I’d like to start with you here and uh then we'd also love to hear from Adam as well for some initial thoughts. But uh where are you seeing the impact of these disparities play out most prominently from your view?
Impact of Health Disparities
[Bridget] Sure first I’d just like to start off by saying thank you for this opportunity.
I have worked in healthcare for more than 25 years in in various capacities and it's just so exciting to see the opportunity for all of the players in our community our health care ecosystem the business to really come together around this discussion on health equity. And I really love the definition that you shared around health equity. It really underscores the importance of us being able to one pay attention and then after we're paying attention listen to what real employee needs are. In this instance and then take the steps to remove the barriers that get in the way of that ideal of optimal health. And so when I think about where we're seeing some of the disparities. We know they're they're many and plentiful and we're seeing them in terms of being able to establish trust. And I wanted to lead with trust because it becomes a true barrier in how people access health care and the confidence that they put in it. And when we have the disparities in African Americans, Latino community members see themselves always you know at risk it kind of limits the trust in the health care system. So that's one way that it plays out.
Another way of course is when we think about wellness. That ideal of maintaining good health on an ongoing and in regular basis and the the thought of well-being. That state of being healthy and and being health happy and comfortable. That's their opportunity to address that as well. So when we think about the workplace we can focus on that ideal of absenteeism and when we're not well we're not going to be at work and contributing to the workplace. And when we're not well our productivity levels go down whether we're dealing with our mental health concerns or we're dealing with managing our diabetes for example. Also, when I think about where it shows up. It shows up in our ability to really understand it and wrap our arms around addressing the drivers of health care. Those things we call social determinants of health and the ability to truly understand how they play out as a whole among our employee population. But then also person by person because there's so many variables and factors that come into play. And then also I will end by focusing on COVID-19 and these last two years and then you know when I say that I I can't believe that I’ve been sitting in my home office for two years.
And when we reflect on that we think about the disparity that came with hope the Corona Virus and COVID-19. And that disparity was seeing the number of the morbidity the number of cases and who they were reflecting afflicting mostly. And then also the mortality associated with that. Who was dying? And here in Michigan for instance we know that in the early months of the pandemic we were seeing disparities of African Americans being more four times more likely to die from COVID and through our education and outreach efforts we were able to bring that disparity down by again providing accurate reliable information and bringing community partners together as well as to employ your capacity as well.
Social Determinants of Health
[Albert] Thank you so much.
[Adam] I’ll just weigh in here too. I’ll say that as stark as these numbers are I am grateful for the conversation today because unfortunately these data are not new. This these realities have been in play for hundreds of years in the United States. And really as uh my colleague said arise from a lot of uh things that are not directly related to health care. Uh she she alluded to the social determinants of health. Then the public health literature really shows that the social determinants of health things like access to education access to transportation, access to healthy food, access to a safe living environment, access to uh you know financial solvency uh those social things such as that really lead to about 80 percent of people's health outcomes. And 20 of people's health outcomes are more directly linked to traditional health care and access as we would normally define it. So given that it's very clear that in order to impact this this takes a change in not just our health system but in our society.
In order to be able to address the structural racism and other factors that have contributed to these social determinants of health and the disparities because they're directly what links to the to the outcomes that we describe.
One clear representation of a social determinant that I like to describe is that of lead poisoning. It's uh I know you've suffered with that a bit in Michigan and lead poisoning is at its core not a health issue it is a housing and water supply issue that reveals itself with a tragic health outcome. So that's a very clear example of a social situation a societal infrastructure problem that reveals itself in a health outcome that is tragic and frankly irreversible and so that that should I think clearly delineate what we mean by a social determinant of health. And again it's not just for along with racial lines the social determinants of health are major influencers in a lot of different areas. Take cancer for example. Where the CDC recently showed that death rates were 14 times higher in rural areas than in urban communities and in urban communities they're higher than they are in suburban communities so it's uh we have a serious problem.
And why is this important from an employer standpoint? Well guess what these are American lives that we're talking about. That are affected here. And they also happen to be your workforce. So it's uh the health of our workforce is key to um the uh the productivity of our efforts and the the health and well-being of our teams and addressing these things becoming informed in these areas is critical for all of us as we move forward and try to improve the outcomes.
Impact of Social Determinants
Yeah, I agree on so many levels and you know really critical especially as you mentioned Adam and Bridget you as well. Just the impact of social determinants and how critical that is to keep in mind and that's certainly something that we see front center as well in our ongoing work at analytics here at the association. As we continue to study issues and identify uh where we're seeing health disparities and deep impacts that you know these social environmental factors can really have uh at a community level or for our members so you know there's a lot to think about here.
On the health care side and in terms of what different employee populations are dealing with uh but would love to also um you know shift gears and also tee uh tee this up for you Amanda. You know let's let's now take a look at how this is hitting the work uh the workplace and how employers are taking notice and looking for strategies to uh address health equity. And you know of course Amanda too would love to to get your perspective on how you're seeing you know a lot of this front center uh play out the most and disparities play out the most prominently from your your view is as well.
[SCREEN TEXT] Slide 3 Impact on the workplace
But um here we have a few data points from SHRM the Society for Human Resource Management recently uh which studied racial inequity in the workplace over a five-year period and found that turnover caused by racial inequity at work may have cost employers up to 172 billion dollars over that time. And that absenteeism caused by experiencing or witnessing racial bias and discrimination at work they account for up to 54 billion dollars in loss. And studies have also estimated the uh cost of health disparities resulting in about 93 billion dollars in excess medical costs which employers may be carrying the brunt of. And uh lastly here 42 billion dollars in lost productivity.
So um Amanda any reactions to this? I mean on the one hand there's a tremendous amount of money that's uh being lost here uh according to what the data is telling us and productivity is mentioned here as well love to hear your thoughts and hear you know you talk about the higher-level impact the result that this can have and what you've been seeing on a workforce in in your business.
What Employers Can Do
[Amanda] Sure yeah it's uh these numbers are really staggering aren't they. They can be very intimidating and I think that um as employers thinking as employers you sort of look at these very structural issues. I um could not agree more with Dr Myers who said that uh you know we're dealing with systemic societal issues as much as we are anything else.
And so as employers I think it can be intimidating and challenging to try to think about how what our place is how can we productively influence this conversation when you look at this massive problem and it is a complex issue. And it's I also completely endorse um what was said earlier about how what we're seeing is not new. You know we're seeing pre-existing trends that are just exacerbated by accelerated by sometimes the pandemic. Um and so I I do think that sometimes it seems insurmountable. We're look we're trying very very hard and I actually think uh to sound a note of optimism I think many employers are trying very very hard to look at these issues squarely. And um I’m not I’m not sure so sure I’m willing to say that it's a silver lining to COVID. Yet I’m not sure that we can really talk about COVID with the silver lining but I I think it has pushed employers to try to confront these overlapping issues.
So what do we do? What do we do as employers? I’ll just offer a couple of things that I think um can be food for thought. For for um for those who are listening or maybe for us to discuss as a panel so first um I think we need to stop thinking about well-being and DEI as programs or as initiatives or as siloed parts of our business. I think that we have to certainly we're trying at our firm and we have to more generally as employers think about well-being and inclusion and belonging as central core management principles that we bring to every part of our organization and try to see our relationship with our employees through the lens of those those two concepts.
Um so I would really encourage um anyone listening to to just to noodle on that because I think that's a powerful idea. When you stop thinking about these things as siloed programs and start thinking about them as um values of organizational values that need to pervade everything. Uh the second thing um I wanted to let me give an example of that because it occurs to me that that's very that might be kind of nebulous.
So we just rolled out a um a very very comprehensive unconscious bias training and I think our time is too short to get too much into what that is. And so I would encourage anyone to Google that if you're listening and wonder um. But but I think we need to think about things like unconscious bias training as well-being programs uh you know that is um the the trying to productively influence the relationships that we have with each other between managers and those who are managed and within this web of relationships that we have within each of our organizations. Um I I think I think that that can be a really helpful view.
Okay so now that I’ve given that example the second thing I wanted to mention um and Bridget alluded to this um is that I think we have to stop thinking about this as a problem that has one solution. There is no one-size-fits-all solution to this these overlapping problems and overlapping issues that present themselves right as health disparities as a lack of health equity.
Um so I think for us at least the we need to try to innovate and educate and try many many different kinds of approaches to address and seek to um remediate this this really complex problem.
So um I think I would want to amplify what Bridget said about going out and listening to your employees. Not every sector of your employee population is going to have the same issues or experience health disparities in the same way and so going out and listening and trying to connect very directly. Whether it's through your employee resource groups whether it's through stay interviews whether it's anything that I think we can do as employers to um to draw that information from our our stakeholders our employees in particular is going to help us in fashioning remedies that are really specific to the underlying problem.
So an example you know when we saw the sort of dual crises of both COVID but also the aftermath of the murder of George Floyd and Brianna Taylor and so many others. Um we we felt like we had to address um that very specifically. The fact that those the linkages between those two things and so we brought in an expert on black mental health in particular to provide um some supportive resources for our our uh employees who are black. And and I think that level of specificity and detail is often going to be necessary in order to correctly identify in a sort of non-paternalistic way the real needs and that's the first step to trying to address them well.
The Challenges
[Albert] That's fantastic. It's interesting, you uh talk about the challenges and also you know the drive to address this and what you've you know just articulated. I really like what you said about you know the need especially to think uh broader and think more holistically around you know how we think about health equity. How we think about diversity equity inclusion and and wellness uh more broadly and make them and embed them as core management principles in our work.
I think that's just so well said uh to build a bit uh on your points you know we we also recently conducted research with business leaders and you know one of them I I uh felt put it really well in painting the scale and the gravity of the challenge that we're up against so so you know I wanted to just highlight this quote here, waiting for the platform to transition but this leader said uh ‘first of all it's the right thing to do, second the issue is so ingrained in all levels of health care that is probably too big of an issue for any employer to tackle by themselves.’
[SCREEN TEXT] Slide 4 “First of all, it’s the right thing to do. Second, the issue is so ingrained in all levels of healthcare that it is probably too big of an issue for any employer to tackle by themselves.”
Building Bridges
Uh Amanda uh turning to you again here just for a second you know this this seems to line up well with what you just articulated. Any reactions this idea of the issue being too big for employers to take on alone.
[Amanda] Yeah I mean I I would absolutely agree with both of the points that that it that this person has stated here and I hope this person is listening so that that he or she can hear hear that um it's clearly the right thing to do. I mean I I don't think that we can really have any kind of pushback on that.
Right this this is just basic fairness um and secondly um that's right I think it's it's these are societal issues and they require a societal response that doesn't mean that we can't work on it. That doesn't mean that we can't try to build bridges. You know we work a lot with our clients um you know we're a huge law firm um and our clients are essentially the fortune 100 and what I see at my firm is is is mirrored in what we see at our clients. You know a sense of caring and an enhanced sense of wanting to take care um and we can work together um we can work with professional organizations for you know in my field. We can work with bar associations um you know. I I suspect that there's many who are listening who have a fairly significant supply chain um you know you can engage with those companies that are within your supply chain to start to try to look at and address these issues. So um I do agree that it's too big for any employer to tackle by themselves but I don't think that we should use that as a reason not to not to start step one.
Health Plan Partners
[Albert] Yeah I couldn't agree more and Adam I’d like to turn to you here as well and ask for your thoughts. And you know how you think health plan partners can support employers and where those partners have to lead.
[Adam] Yeah I think there's a lot of ways that we can support and one of them is the call for new and better data. It is only recently and we still have a long ways to go that racial uh ethnicity and language data are gathered with any sort of consistency in the medical record. So if they're not gathered in the medical record how can you explore and study them as factors that potentially contribute. The same goes for social determinants of health data. Only recently I would say in the last two years or so have health systems begun to figure out how can we reliably collect these data as well do people who are trusting us with their care have the food that they need? Do they have safe and affordable housing? Are they in a safe environment free from domestic abuse or violence? Do they have um you know reading difficulties? Do they have all kinds of struggles that are very real and very impactful for people's health outcomes that those were just simply data that weren't captured before and only now are people beginning to capture them and then importantly factor them into treatment plans with an eye toward mitigating those social struggles in addition to just treating the quote-unquote traditional disease state.
So I I think part of that is partnering on those data and encouraging employees and our staff to be forthcoming about self-reporting on those things to their health care providers is I think important. And again that's a difficult thing and there's trust barriers that exist that are very real and frankly quite earned in the healthcare system that we have to overcome. But I think only as we get these data can we lean in quite a bit you know there's a lot that we can do.
[SCREEN TEXT] Slide 5 The BCBS National Health Equity Strategy will confront the nation’s crisis in health disparities
We have a national health equity strategy that we'll touch on in greater detail later uh but you know the part of that has to do with focusing on impacting maternal health and and doing so by sharing this implicit bias training for providers. We partnered with the March of Dimes and made implicit bias training their implicit bias training which is uh wonderful. Available to 1.7 million credentialed clinicians across the Blue system that they can take this free of charge we're going to be leaning in on diabetes and cardiovascular conditions as well as the important stigma and struggles that people have with behavioral health.
One of the data points that you shared early on Albert was that people who are in minority uh communities uh suffer unnecessarily and in a disparate way from undiagnosed and untreated behavioral health struggles. That's a crime. And we are only when we are looking at these data and working together to impact them. Can we do that? And part of it is going to be data as I’ve described some of us can be scaling best practices and programs that have worked.
I’ve talked about unconscious bias but also activating new and creative public private payer provider community partnerships at a at a local level. This is a national problem that will get solved at both the national level and the local level and it can seem overwhelming to think about it given all of the different factors involved but I like to say that we we cannot do this alone. But we each alone can do our part so if we each plug in and do our part then in aggregate together we'll move the needle.
[Albert] Yeah that's uh very well said Adam and I appreciate you talking a little bit about some of the thinking in the action that's already under underway across the Blues. It's certainly uh work and a topic that's been near and dear to my heart. And so many of others at the association and across our Blue plans.
Bring Humanity Back
So you know um but with this in mind I’ll ask Bridget here first and then perhaps also some follow-up uh from from you Adam just given what you just shared just now but the question I have here is what other ways do you see health plans and employers working together to advance health equity.
[Bridget] Yeah so i want to go back to something that Amanda said that really fits into this. And I think when we look into our workplace community we have the opportunity to bring humanity back that means recognizing that each person who walks through that door that they're a person a human being. And being able to recognize what their unique needs are is key and when we talk about diversity equity and inclusion. And I always say these are really big words the opportunity there is to break that down and define that diversity is not just about race it's really again about that opportunity to recognize the different dimensions of a person.
So when we think about wellness and well-being and addressing health and health care disparities and I always separate the two on purpose um and I’ll define them in a minute um there's an opportunity to really be spit specific and personalize health care and health care delivery to degree and i always separate health and health care disparities because they're truly two different things a health disparity refers to those outcomes that we see disproportionately towards a certain population in our community and again it's those health outcomes when we think about diabetes and we already saw the statistics around that that's the health outcome but when we think about health care disparities it's that reflection on things like access and the coverage. And so as employers you can think about the kind of coverage that we provide um for our employees. And then another opportunity is around health literacy where I see it's a great opportunity for people to come together the plans and the employers to to really make sure that we're communicating in a way that's clear and simple. That we're communicating in a way that's culturally competent and is reflective of the individuals we're communicating to. That we're providing clear instruction and information on resources that are available in the community and how to access those resources. We've heard the saying it takes a community or a village right? it takes a village and it's really true in this situation. There's no silver bullet as I mentioned at the start of this I’ve been working in healthcare in different roles for 25 years. And we're still trying to solve same issues. What's exciting is that now we're really coming together and we're engaging in this dialogue. And as we engage in this dialogue that's the opportunity for us to share the the best practices. And I’m really excited about the work that we're doing in alignment with the Blue Cross Blue Shield association around our health equity strategy. And we have five primary focus areas um we're focusing on primary care access the quality of that health care is that's delivered. And in 2020, we launched our unconscious bias education for primary care providers and the staff in their office because we have to think about when an individual walks into that doctor's office what is their immediate experience? How are they received? Are they received in a culturally sensitive and appropriate way for example. Do we take notice that they may be a member of our deaf and hard of hearing community so all of these things are important to pay attention to and develop that self-awareness in the delivery of care we're also focusing on behavioral health, maternal health, looking at chronic disease prevention in general as well as health promotion. A lot of that is through working with employers and working with community organizations to get again accurate and reliable information about the various health concerns and prevention of those health concerns. And when we talk about COVID we did a lot with COVID we did everything from address and food security that increased over these last two years even more than it was to getting information about where you can go for testing. Helping to get testing in local neighborhoods and communities. So there's access and then when it comes to the vaccine the same issue giving it to where people have access to the vaccine. So we're not seeing disparities in terms of who's getting the vaccine because there's no access and who's not.
Um so those are just some of the ways that we have partnered with our employee community. And I must say that we worked with a group customer as well around addressing unconscious bias. We had dialogue. We were talking about what the needs are and together we came to that conclusion that this is one area we need to strongly focus on.
So again, I’m going to circle right back to the point that the more we have dialogue and the more we share best practices and we're listening and we're deepening our understanding we're going to come up with solutions that can truly move the needle. And I’m that just excites me so much. Um as I look into the future and I see a bright light I’m an optimist but I’m going to keep doing this right live and you know it's moments like this that really encourages me in the work that we're doing.
Be a Part of This Change
[Albert] I love your optimism I I share the same sentiments and I think you you have to do. You have to be uh to work in this industry um and uh you know be a part of this this change that I think we're really on the cusp of. Um Adam any additional thoughts you'd like to share here too?
[Adam] Yeah I think you know I’ll echo many of the things that uh that Bridget shared but I’ll double click on one piece of it she used the word prevention our health system and our approach to health care in the United States is really more one of disease care than it is of health care it's treatment of disease rather than promotion of health that's the way it historically has been in the US. It is not that way in all countries um and in fact you know I think that is if you study it that is in part one of the reasons why our health care spend as an industrialized nation is number one out of the top 11 industrialized nations and we are number 11 in outcomes amongst the top 11 industrialized nations.
So number one in spend by far number 11 in outcomes that matter. In very basic important things like life expectancy. So that's partly because of our focus on the downstream. And so to the degree that you as employers can partner with health plans and others about focusing on promoting health promoting well-being promoting prevention amongst your teams then I think that will help change that paradigm quite a bit.
Top of Mind for Employers
[Albert] I totally agree and you know thank you both you know Bridget, Adam for for sharing your thoughts here. And it's actually a good segue into our next section.
Um so let's actually go into the topic of what's top of mind for employers a little deeper and you know discuss what we see companies and their business leaders already doing.
[SCREEN TEXT] Slide 6 Impact of COVID-19 on Large Employers’ Health and Well-being Priorities, 2021
I’ll um just bring in this study here by the business group on health an association of benefit experts and large employer members. You know they looked at what companies were prioritizing in light of the impact of the pandemic and and how they potentially accelerated certain priorities as a response. And you can see here just right off the bat improving mental health access and services, expanding virtual health services, and and promoting health equity in terms of increased focus areas really rose to the top.
So Amanda here uh what are your thoughts that's what seems to be rising to the top um based on the insights from this BGH survey any reactions to this from your point of view?
[Amanda] So yeah I mean I I think this is entirely consistent with what we're seeing ourselves and also what we're seeing with our clients. The one thing I will say though is that while accurate I’m not sure it completely tells the whole story. My very strong suspicion is is that the first metric measured and the last are actually seeking to get at the same thing right? That um you know there are disparities in mental health access and services that we we know they're there. Um the science is very clear.
So corporations who are promoting health equity are will be seeking to improve access, mental health, we've been talking about access Bridgette was talking about that as as being one of the key things that employers I think both both of my fellow panelists were talking about those things as the the a very a very interesting way for and productive way for employers to get involved in this conversation and work on this problem is to to reduce barriers to access. And um so I suspect that's what's that's happening here is that as we're focusing on health equity we're focusing on focusing on mental health access. And vice versa.
[Albert] Right I agree with you and I think uh just that more holistically. Yes, I think is is a better picture of what's going on here. Bridgette do you have uh any thoughts here from your perspective?
[Bridget] Yes definitely good things came to mind just now and is reflecting what you brought up earlier Amanda about the events of 2020 um from the murder of George Floyd to the global response that we saw. And since that time just all of the national tragedies that we have experienced so we can even equate this to all of that beyond COVID-19. So I kind of wanted to lift that up because we know that even though many of us are still working remotely that we're bringing all of these into the workplace for that call and that need to improve mental health services key.
But another piece is that as we think about that I’ll add on in terms of that equity piece that when we think about expanding virtual health services making sure we ask the right questions about the ability of all employees to be able to assess that and and with ease and and what that looks like. And then that opportunity to um really understand when we're creating that access you know what do the practitioners look like? And Albert I want to try to recall from that recent information um from the behavioral date health data that you all just shared at the association about African Americans in particular. They feel most comfortable with a health care pro a behavioral health care professional who looks like them. And we know that across this nation that there is a gap there. But it's also something we have to keep in mind we have to consider when we think about these services. So it's one thing to provide the service, but it's another thing and a very important thing to make sure that we're providing the services in a way that meets the needs of employees.
Education and Training
[Albert] Yeah I couldn't agree more and uh you know also appreciate you you know bringing up teeing up our work that was uh pushed out recently. You know I I want to pivot a bit here by you know acknowledging that you know we're talking a lot about access which you know certainly agree is absolutely critical, but to take this even further and the question that's coming to mind for me that I think will help frame this uh next section of our discussion here is you know. What beyond improving access to employers need to focus on? One thing we've been mentioning along the way is education um I from my view I’d also pair that with training right?
Um one thing that I think would be important impactful to our audience to talk a little bit more about them is you know how this ties into um you know cultural competency. And Bridget you know I’ll pick on you here again but I’ll mention you know I mentioned your focus on cultural competency. In your role as part of our introductions at the top of our hour um i want to read a quote of yours here that I found to be compelling and relevant to this topic. Um you know I read where you said, quotes at Blue Cross Blue Shield of Michigan we are on the path to cultural competency, a place where there is understanding and acceptance of differences uh as well as similarities.” What I really like is that you know you say you're on a path to cultural competency what does it take to get cultural competency?
Cultural Competency
Well first of all it's a lifelong process. I’ve worked in um again healthcare working with many communities many different communities and learning to understand what their needs are. And I’ve worked in inclusion and diversity for six strong years but I’m still on a journey. I’m still on the path to developing cultural competency. And so I would start there with the fact that it's lifelong.
And what it involves is the opportunity to remove ourselves from our normal circumstances. I live in metro Detroit and metro Detroit is actually one of the most segregated communities in the nation. And I think it's going to be modeled in a lot of other communities. So we go to work, we interact, and we interface with others who may look different from us on the outside. But then we go back home to our communities where most of the people are going to look just like ourselves. And so that's the opportunity to remove ourselves and immerse ourselves in environments and communities that is not our norm, that looks different from what we're accustomed to. And that's what we're going to expand I call our consciousness. That ability not to see something as different or foreign or you know I’m uncomfortable with it because that's where the unconscious bias comes into play. And as human beings we all have it. So I always like to say that, but like we're in the um the provider setting for example it can show up due to weight issues or views we might have about the LGBTQ plus community.
Again um stereotypes and assumptions we may have about African American women. But the more that we expose ourselves and learn about those different communities learn their differences this because there's richness there, but then also the similarities. It's going to be less of a foreign ideal or a concept where we're going to be more mindful in our interactions. And we're going to recognize that the person across for me is not someone so different from me. Or, I hold this stereotype for the person. The person across from me is a human being with their own unique needs in terms of health care. And I’m going to focus on and prevention because we really got to move from that place of sick being the norm. Sick is not the norm. Wellness and well-being is different.
Um so at Blue Cross Blue Shield for example and I I’ll wrap it up here is that it is the cultural competency is the cornerstone of in the foundation of everything that we do around English and adversity. It's required education for our employees. So as new hires come into the company they have to go through this learning session. And we continue to build on that every year with over 100 learning sessions. We cover the spec from different cultures communities generations that's important.
If we think about everything from senior sensitivity to just recognizing um again the similarities and differences in the nations. Um looking at different work styles and different perspectives so all of those come into play. When we're talking about the workplace community in general and learning about what they're need and also when we're talking specifically about how we deliver health care or how we do develop health care policy. So that's important too and so we have to be mindful of the bias even when we're developing policy. As Dr Meyer shared earlier this is systemic a lot of what we see is systemic. And we have to pay attention to the programs and processes and policies that we're putting in place that sometimes lead to these disparate outcomes you see.
Steps Employers Can Take
[Albert] Yeah all excellent point points and I totally agree. um you know Amanda and
Adam also point the a follow-up question here to you. Are there specific things that you think employers can do or steps they can take to promote a culturally competent workplace?
[Amanda] Yeah I mean absolutely I’ll jump in. Um you know I think the biggest thing that we can do right now is I think Bridget was alluding to this is understands art understand ourselves as employers whether you're in HR, whether you're in the C-suite whether you whatever part of the organization that you're in that you are in a process of continuously educating yourself about about cultural competence because culture itself is evolving right? Um you know all of our norms are changing. And that's great that's good we're on you know hopefully on that arc towards a more sort of equitable society. Um so I really do think that um that education is important. And if you're in a position where you feel like your management could benefit from education you have the ability to put some of these things in front of management right? Those very intimidating numbers that we talked about earlier? About how much these health disparities are a drag on productivity. How much they're costing employers. That's really good information to get in front of management in order to make the case that there is a role for employers. Um working within this larger community to try to address some of these issues that we've been discussing.
Challenges Employers Can Take
[Adam] Yeah I would echo so much of what uh colleagues have said. And I’ll stress a couple things. In fact I’ll issue a little bit of a challenge to employers frankly to all of us would be to look internally at ourselves and our own policies and procedures. Policies and procedures around a variety of different things. Our hiring policies and procedures. How we interview versus don't uh our policies around you know tardiness to the workplace and things like that.
I mean if you have significant portions of your workforce that are dependent on public transportation that is implicitly less reliable maybe than transportation that is private uh you you know? Do you have some sort of grace involved that allows people who have that challenge to to occasionally be be tardy? Uh remote work uh opportunities. Not everyone has access to high quality broadband the digital divide is real and COVID made that even more clear when the digital divide to at home work at home school and at home remote health care became very very real and further created disparity.
So are there ways that you internally as you have remote workforce can you promote accessibility to work through uh things like hot spots etc. But then I would also even basic things I would challenge the teams to think about even when you schedule your meetings are you scheduling your meetings at those critical hours when families are
transitioning with children and with loved ones etc. If so and you're scheduling your critical meetings at those times, are you inadvertently excluding people who might be more female or might you know have more responsibility for those family issues from the conversation. And so even on sort of a very granular level like that I think there's opportunity for improvement so that's where I’ll pause.
[SCREEN TEXT] Slide 7 Top three actions employers should focus on now
[Albert] Right so it's you know we can see from the perspectives our panelists have shared here there's plenty for all of us to work on to address such a systemic problem. Um just doing a quick time check here let's wrap this section of our discussion before uh before we get to Q&A by summing up some of the specific strategies we've covered just briefly. And here are a few things that we've discussed where employers can start. Number one collaborate with your health plan partner on practical ways to improve access and crucially consult with them on how to educate leadership about health equity to obtain the right level of buy-in and involvement at the top.
Secondly create flexibility when it comes to time off PTO work scheduling and leave for health needs like vaccinations, preventive screenings, doctor visits, behavioral care or consider bringing services on site.
And finally listen to diverse groups of people and meet with employee resource groups to better understand the needs and address barriers for employees across your workforce. Just as Adam articulated just a few minutes ago and we talked about. All kinds of things from certain populations having trust issues with providers to uncovering internal policies or practices that may be negatively impacting certain groups.
[SCREEN TEXT] Slide 8 Q&A
Um so you know I’ll go ahead and bring us to since we have seven minutes remaining just you know open things up for for Q&A. And uh you know I’d like to just start off here checking the the Q&A uh panel here of our platform. Uh we have a couple questions but just to start off with here um you know and feel free anybody on our panel here to start but uh what mechanisms have you found effective for soliciting employee input on this topic and the unique needs of uh excuse me specific employee populations.
Employee Resource Groups
[Amanda] I can jump in here sorry go ahead.
[Bridget] I think I was just going to build on that concept of the value of employee resource groups. We call them networks that Blue Cross Blue Shield of Michigan um and the the opportunity to really use those groups of uh community to get some insight about what those issues are. You would be amazed at how there's such great feedback that comes back through those conversations and dialogues. Um we have one that's called Bright Blue employee resource network that focuses on on seen and unseen disabilities and it provides a wealth of information. We have another equally Blue that focuses on the LGBTQ plus community. And I really lean on them to kind of be my eyes and ears in terms of what we need to understand better about serving this community especially as it relates to transgender needs for example. So I think those have been very effective for us as a health plan working in partnership with employers for example.
Humility
[Amanda] Yep I agree I was gonna I was gonna talk about ERGs too. It's all about relationships right? You have to sort of get in there and know and and approach it. I think um with humility right? With that this this concept that every we're all continuously learning and um we might make mistakes but we have to um we have to sort of embrace embrace change. And um and and operate as if we're all on the same team right? That we're all trying to sort of make it a better more inclusive workplace a workplace where people are thriving not just not just um you know existing in a place where where they aren't sick instead they're thriving. That's what we're pushing towards.
Question
[Albert] Gotcha that totally makes sense. Um we do have a question that's come in from a friend of ours at Blue Cross Blue Shield of North Carolina. Um you know she asks
when when large employers are promoting health equity, what exactly does that entail? And um I’m sure there's a lot that comes to mind for both of you Bridget and Amanda but uh feel free to jump in. I’ll let you go first this time in America.
[Amanda] So um I wish that there was a single sort of cookie cutter response to that. I think that there's a lot of different approaches that an employer could take and many of them are going to be worth doing. Um so you know and and they may vary what does your population look like? You know do you have a population that happens to be mostly women employee population. I mean you know where are you geographically. Do you have um you know what do you know, um about your employee population that can help you pick a strategy right? Are most of your employees um uh over the age of 60? Are most of your employees do they have children young children? You know I think that there's a lot that you can do because health equity issues or health disparities rather um can can have many different forms. So um I think you start by educating by educating yourself right? Um looking inward I think Adam you said that right? That you need to look inward um at your own population trying to learn about your own organization.
And then there are enormous resources including the amazing e-magazine that I just want to point out um was was just developed. I I think that that's a a great place to start and you can sort of build from there. In thinking about strategies the only thing I would say is that I would not limit yourself to one strategy. Prepare to sort of try multiple things have them not necessarily work out exactly the way that you want but you know fail forward. Uh be able to sort of learn continuously as you try to seek out the things that might be helpful and get that get that positive feedback loop going so that you know whether or not things are working.
Adams Answer
[Albert] Right and I want to squeeze in one more question.
[Bridget] And uh I’m ready to respond to that question, real quick. We want to maximize your time we're flowing out um down because they were just filling it out so quickly. I would just start with um one if I were an employer I would start with promoting the fact that sickness is not the norm. And then from there I would focus on that ideal of achieving optimal health. That what do we need to do what does that mean? How do you break that down and then when I think about my employees in my company I would think about how I can help them promote balance in their lives.
Again big term but you break that down in terms of what that really means and then help to connect the employees to community resources. As Dr Meyers pointed out earlier when we think about the contributors and the drivers of healthcare you know 80 are the social factors that are outside the walls of our workplaces. And so that's how I if I were an employer would approach it cast that vision and then start breaking it down in ways that's going to connect with employees
Closing
[Albert] Appreciate you sharing um you know. Adam, I just want to squeeze you in here any room any thoughts to build on what Bridgette, Amanda shared here before we close out?
[Adam] I think they've covered it very well. It's uh it's going to take a lot of different sustained strategies to do this again but it's important work and uh grateful for the opportunity to have the dialogue today. You can feel free to reach out to us again I saw there were other questions in the chat room and we will we can connect with you directly if you'd like on those.
[Albert] All right thank you so unbelievably we're already closing in uh on the end of our time today. I want to thank everyone for tuning in to be a part of this discussion. I hope you've gotten as much out of this as I have during our very quick one hour that is of course one webinar in more conversations coming in the future keyed in on the topic of health equity.
I want to extend a very special thanks again to my fellow panelists and for our audience. I hope you'll keep the conversation going with your colleagues your health plan partners and others that you work with and I hope you'll take it from there into implementing solutions that drive change and advance health equity for your workforce.
For more information on advancing health equity remember to check out our latest mini e magazine and other resources at smarterbetterhealthcare.com. Thank you everyone for tuning in today we wish you and your families a very happy and safe holiday season and we we look forward to connecting with you again in the new year. Take care and we'll see you again soon.
Point of Blue
See the latest Blue Cross NC tips, news and community updates in our blog.

One woman helping many communities
Helping rural communities heal who face higher rates of childhood trauma.

Black leaders on whole-person health
They're supporting their communities on the journey to joy.
Find an employer plan
Ready to learn more about employee coverage options? Whether you manage the benefits for thousands of employees or just a handful, we have a plan for you.
Disclosures:
-
Turner, Ani. The Business Case For Racial Equity: A Strategy For Growth. Altarum/W. K. Kellogg Foundation: July 24, 2018. Online: www.wkkf.org/resource-directory/resources/2018/07/business-case-for-racial-equity (Accessed January 2022).
-
Tori B. Powell, “Black Women Are at Higher Risk for Miscarriage, Study Finds,” CBSN, Apr. 29, 2021. cbsnews.com/news/miscarriage-risk-black-women/ (Accessed July 2023).
-
Young-Mee Kim, PhD, and Sung il-Cho, PhD, MD, “Socioeconomic Status, Work-Life Conflict, and Mental Health,” American Journal of Industrial Medicine, May 17, 2020.
All other trade names are the property of their respective owners.
U38960, 7/23
Blue Cross and Blue Shield of North Carolina does not discriminate on the basis of race, color, national origin, sex, age or disability in its health programs and activities. Learn more about our non-discrimination policy and no-cost services available to you.
Information in other languages: Español 中文 Tiếng Việt 한국어 Français العَرَبِيَّة Hmoob ру́сский Tagalog ગુજરાતી ភាសាខ្មែរ Deutsch हिन्दी ລາວ 日本語
© 2024 Blue Cross and Blue Shield of North Carolina. ®, SM Marks of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield plans. All other marks and names are property of their respective owners. Blue Cross and Blue Shield of North Carolina is an independent licensee of the Blue Cross and Blue Shield Association.