Description of Procedure or Service
Definitions
Cystic fibrosis (CF) is an autosomal recessive genetic disease in which dysfunctional epithelial chloride channels lead to excessively thick mucus affecting multiple organ systems. Common complications include mucous plugging of the airway, lung inflammation, chronic pulmonary infections, intestinal malabsorption, pancreatic insufficiency and infertility (Pritchard, 2016).
***Note: This Medical Policy is complex and technical. For questions concerning the technical language and/or specific clinical indications for its use, please consult your physician.
Policy
BCBSNC will provide coverage for genetic testing for cystic fibrosis when it is determined to be medically necessary because the medical criteria and guidelines shown below are met.
Benefits Application
This medical policy relates only to the services or supplies described herein. Please refer to the Member's Benefit Booklet for availability of benefits. Member's benefits may vary according to benefit design; therefore member benefit language should be reviewed before applying the terms of this medical policy.
When Genetic Testing for Cystic Fibrosis is covered
Testing for CFTR mutations is considered medically necessary only once per lifetime.
- Carrier screening for cystic fibrosis, using a panel containing mutations proven as causative of CF (as defined by the CFTR2 project) and including the ACMG-recommended panel of the most common mutations (see Policy Guideline #1 below), is considered medically necessary in all of the following situations:
- For all pregnant women OR
- For all women seeking pre-conception counseling OR
- For individuals who have a family history of cystic fibrosis or have a first degree relative who is a known carrier of cystic fibrosis.(Testing needs to include any known familial mutations if not already included in the panel) OR
- For the male reproductive partners of women who have been identified as cystic fibrosis carriers OR
- For the reproductive partners of individuals diagnosed with cystic fibrosis OR
- Testing of a fetus for mutations in the CFTR gene (including all known parental mutations) is considered medically necessary when:
- Both biological parents are cystic fibrosis carriers
- One or both biological parents are affected with cystic fibrosis
- One biological parent is a cystic fibrosis carrier and the other parent is not available for testing
- Echogenic bowel is detected by fetal ultrasound
- Testing for mutations in the CFTR gene, using a panel containing mutations proven as causative of CF (as defined by the CFTR2 project) and including the ACMG-recommended panel of the most common mutations is considered medically necessary in order to make the diagnosis in a newborn or confirm the diagnosis after an abnormal newborn screening result using immunoreactive trypsinogen.
- Testing for mutations in the CFTR gene is considered medically necessary as an adjunct to sweat testing in individuals presenting with symptoms of cystic fibrosis, as follows;
- When there are known familial mutations, testing needs to include the familial mutations.
- When there are no known familial mutations, or if only one familial mutation is known, testing needs to be done with a panel containing mutations proven as causative of CF (as defined by the CFTR2 project) as well as include the ACMG-recommended panel of the most common mutations. If the known familial mutation is not included in that panel, then testing for the known mutation needs to be performed additionally.
- Sequencing of the CFTR gene meets coverage criteria if no mutations or only one mutation are found using the above panel, and the clinical suspicion of cystic fibrosis remains.
- If sequencing of the CFTR gene does not reveal two disease-causing mutations, and the clinical suspicion of cystic fibrosis remains, testing for deletions and duplications in the CFTR gene meets coverage criteria.
- Testing for mutations in the CFTR gene, using a panel containing mutations proven as causative of CF (as defined by the CFTR2 project) and including the ACMG-recommended panel of the most common mutations, along with testing for the IVS8 5T/7T/9T variant, is considered medically necessary in males with CBAVD. If mutations are not detected with the standard panel, and a diagnosis of cystic fibrosis related CBAVD remains a consideration, sequencing of the CFTR gene meets coverage criteria.
- Testing for the IVS8 5T/7T/9T variant is considered medically necessary for cystic fibrosis carrier screening only as a reflex test when the R117H mutation is detected on carrier screening.
- Genetic Counseling is considered medically necessary for:
- Individuals found to be cystic fibrosis carriers
- Individuals with a diagnosis of cystic fibrosis
- Individuals with a family history of cystic fibrosis
- Individuals who are the reproductive partner of a cystic fibrosis carrier
- Individuals who are the reproductive partner of a person diagnosed with cystic fibrosis or CBAVD.
Policy Guideline #1: A core panel of 23 mutations are recommended by the American College of Medical Genetics (ACMG) is considered medically necessary for cystic fibrosis genetic testing. The standard mutation panel is as follows:
- ∆F508
- ∆I507
- G542X
- G551D
- W1282X
- N1303K
- R553X
- 621+1G→T
- R117H
- 1717-1G→A
- A455E
- R560T
- R1162X
- G85E
- R334W
- R347P
- 711+1G→T
- 1898+1G→A
- 2184delA
- 3120+1G→A
- 3849+10kbC→T
- 2789+5G→A
- 3659delC
When Genetic Testing for Cystic Fibrosis is not covered
Sequencing of the CFTR gene is considered not medically necessary for cystic fibrosis carrier screening.
Policy Guidelines
Background
Cystic fibrosis is a common life-limiting autosomal recessive genetic disorder, caused by mutation of a gene that encodes an epithelial chloride-conducting transmembrane channel called the cystic fibrosis transmembrane conductance regulator (CFTR), which regulates anion transport and mucociliary clearance. The CFTR protein was first identified as a chloride channel, but has been shown to facilitate or regulate the transport of other ions, such as sodium, thiocyanate, bicarbonate, as well as water absorption and excretion (Clancy & Jain, 2012; Cohen-Cymberknoh, Shoseyov, & Kerem, 2011). The CFTR protein is present in the epithelia of various tissues, including that of the lungs, sweat glands, gastrointestinal tract, vas deferens, and pancreas (Barrett, Alagely, & Topol, 2012). CFTR dysfunction mainly affects epithelial cells, although there is evidence of a role in immune cells.
Mutations in the CFTR gene which impede protein production, stability, or activity, result in less available functional protein (Clancy & Jain, 2012). Functional failure of CFTR results in defective mucociliary clearance, chronic infection and abnormal inflammatory response which lead to progressive, irreversible lung damage (Cohen-Cymberknoh et al., 2011). Other manifestations of dysfunctional CFTR include pancreatic insufficiency, meconium ileus, and congenital bilateral absence of the vas deferens (Barrett et al., 2012; Schechter, 2014). The early identification and treatment of patients by multidisciplinary teams have resulted in improvements in both quality of life and clinical outcomes in patients with cystic fibrosis, with median life expectancy now over 40 years (Pritchard, 2016; Schechter, 2014).
Most mutations of the CFTR gene are missense alterations, but other mutations, deletions and insertions have been described (Bell, De Boeck, & Amaral, 2015). To date, over 2000 mutations have been identified in the CFTR gene (CF Foundation, 2017). CFTR mutations can be divided into six classes according to their effects on protein function (Boucher, 2010; Elborn, 2016; Wilschanski et al., 1995).
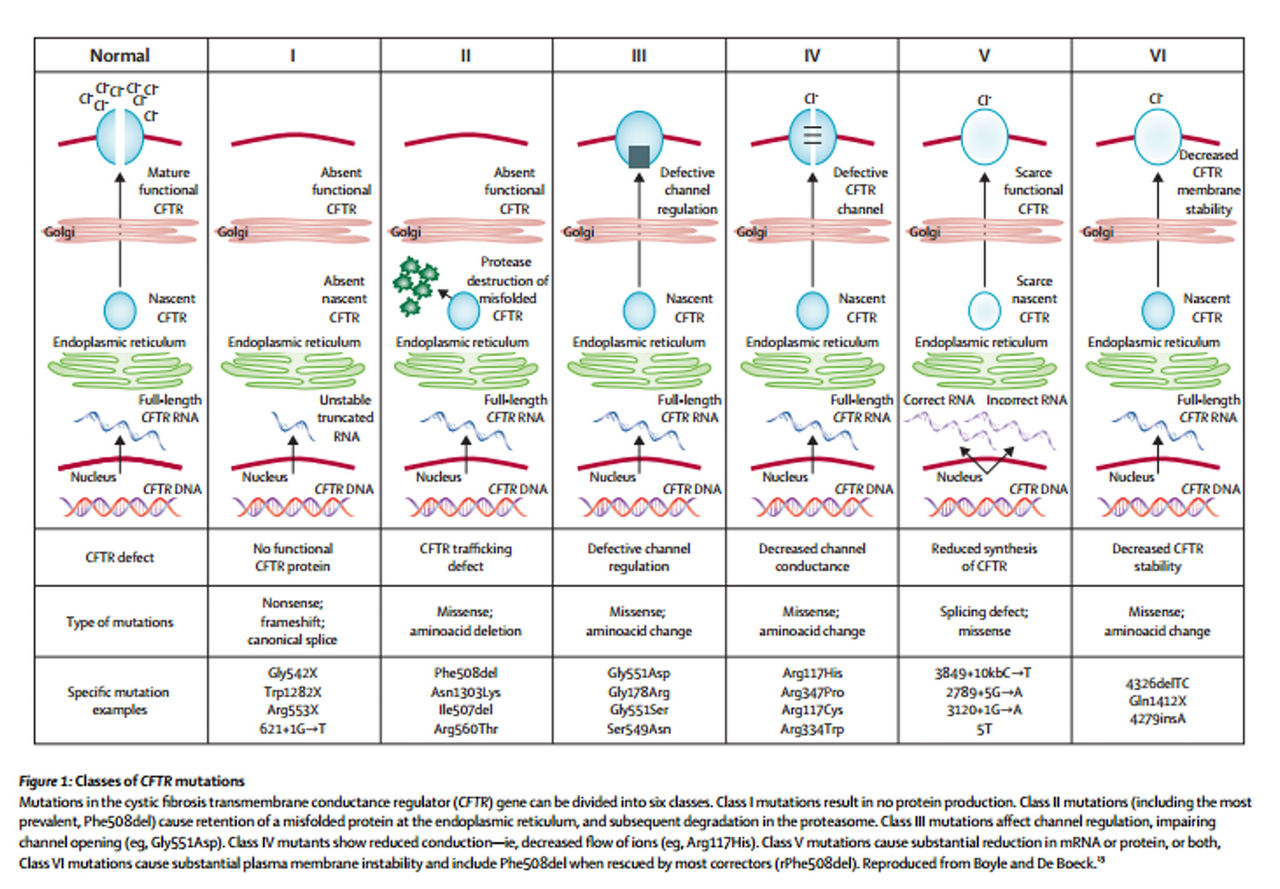
From:(Elborn, 2016)
Class I, II, and III mutations are associated with no residual CFTR function and patients with these mutations have a severe phenotype, whereas individuals with class IV, V, and VI mutations have some residual function of CFTR protein and have a mild lung phenotype and pancreatic sufficiency (Elborn, 2016; Wilschanski et al., 1995).
Clinical Validity and Utility
Because of the relatively high frequency in the U.S. population and studies demonstrating that early detection and care can improve outcomes, CF testing is included as part of the newborn screen in all states (Grosse et al., 2004). Newborn screening (NBS) for CF can include testing for immunoreactive trypsinogen (IRT), which is a pancreatic enzyme found at elevated levels in the blood of some individuals with CF; genetic testing for common CF mutations; or a combination of IRT and genetic testing. Positive newborn screens are typically followed by genetic testing (if not already done), and a sweat test, which measures the chloride concentration in sweat. The sweat test historically has been considered the “gold standard” for CF diagnosis. The presence of 2 disease-causing mutations also may be considered diagnostic of the disease, even in the absence of classic symptoms or in the case of a negative or inconclusive sweat test (Farrell et al., 2008).
In addition to NBS, CF carrier screening (PCS) has become commonplace in the U.S., particularly among pregnant women and couples planning a pregnancy. PCS has been found to markedly reduce CF birth rates with a shift towards milder mutations, but was often avoided for cultural reasons necessitating the use of complementary PCS and NBS (Stafler et al., 2016).
A subset of 23 mutations accounting for the majority of cystic fibrosis cases in the U.S. and were accepted by most guidelines as the primary genes to be screened for diagnosis of CF and carrier status. The most common CF-causing mutation is F508del, which is present in over 70% of known CF cases. The Clinical and Functional Translation of CFTR (CFTR2) project continually evaluates genotype and phenotype correlations and has confirmed many additional mutations as being causative of CF (CF Foundation, 2017). Information from over 88,000 patients with specific cystic fibrosis variants from the United States, Canada, and Europe was collected by the CFTR2 team from national CF Patient Registries and placed in the CFTR2 database, and then developed CFTR2 website which contains information about the 322 most common CFTR variants (CF Foundation, 2017).
Analysis of data from the CF Foundation Patient Registry found that patients of Hispanic, black, or Asian ancestry were less likely to have two identified CFTR variants, and more likely to carry no mutations on the commonly used 23 mutation carrier screening panel (Schrijver et al., 2016). Analysis of the Exome Aggregation Consortium dataset also found that none of the current genetic screening panels or existing CFTR mutation databases covered a majority of deleterious variants in any geographical population outside of Europe. Both clinical annotation and mutation coverage by commercially available targeted screening panels for CF are strongly biased toward detection of reproductive risk in persons of European descent (Lim et al., 2016). This research indicates the possible need for adjustment of this panel to facilitate equity in mutation detection between white and nonwhite or mixed-ethnicity CF patients, enabling an earlier diagnosis improving their quality of life.
The integration of next generation sequencing into CF diagnostic protocols has also begun to be examined. A diagnostic protocol in which a quick and relatively low-cost PCR-based screening for the most common CF mutation, F508del, followed by full-gene next generation (NGS) sequencing of CFTR was shown to improve genetic diagnosis and holds promise to be a straightforward, convenient and rapid diagnostic protocol for CF patients (Straniero et al., 2016). A study of using NGS in for NBS found that the NGS assay was 100% concordant with traditional methods. Retrospective analysis results indicate an IRT/NGS screening algorithm would enable high sensitivity, better specificity and positive predictive value (Baker et al., 2016).
CFTR modulators are a new class of medications targeting the underlying defect in CF by improving production, intracellular processing, and/or function of the defective CFTR protein. Ivacaftor (IVA), which improves chloride channel function, IVA combined with lumacaftor (LUM), which partially corrects the CFTR misfolding, and IVA combined with tezacaftor, which improves the intracellular processing and trafficking of CFTR, have been approved by the U.S. Food and Drug Administration for use in patients with CF. The indications and efficacy of these drugs depend upon the CFTR mutation in the individual patient. Therefore, all CF patients should undergo CFTR genotyping to determine if they carry a mutation that makes them eligible for CFTR modulator therapy (Simon, 2018).
Applicable Federal Regulations
On March 28, 2006 the FDA (2006a) approved eSensor Cystic Fibrosis Carrier Detection System as a device for the detection of carrier status for cystic fibrosis for all adult couples contemplating pregnancy, regardless of ethnicity. It is a qualitative genotyping assay that simultaneously detects mutations currently recommended by the American College of Medical Genetics and American College of Obstetricians and Gynecologists (ACMG/ACOG). The eSensor® CFCD System is not indicated for prenatal screening or to establish a diagnosis for cystic fibrosis.
On June 7, 2006 the FDA (2006b) approved Tag-It™ Cystic Fibrosis Kit as a device used to simultaneously detect and identify a panel of mutations and variants in the cystic fibrosis transmembrane conductance regulator (CFTR) gene in human blood specimens. The panel includes mutations and variants currently recommended by the American College of Medical Genetics and American College of Obstetricians and Gynecologists (ACMG/ACOG), plus some of the worlds most common and North American-prevalent mutations. The Tag-It™ Cystic Fibrosis Kit is a qualitative genotyping test which provides information intended to be used for carrier testing in adults of reproductive age, as an aid in newborn screening, and 2 in confirmatory diagnostic testing in newborns and children.
On September 9, 2007 the FDA (2007) approved Cystic Fibrosis Genotyping Assay as a qualitative in vitro diagnostic device used to genotype a panel of mutations and variants in the cystic fibrosis transmembrane conductance regulator (CFTR) gene in genomic deoxyribonucleic acid (DNA) isolated from human whole blood specimens. The panel includes mutations and variants recommended by the American College of Medical Genetics (ACMG, 2004) and the American College of Obstetricians and Gynecologists (ACOG, 2005) plus additional multiethnic mutations.
The Cystic Fibrosis Genotyping Assay provides information intended to be used for carrier testing in adults of reproductive age, as an aid in newborn screening and in confirmatory diagnostic testing of newborns and children. This test is not indicated for use in fetal diagnostic or pre-implantation testing. This test is also not indicated for stand-alone diagnostic purposes.
On March 13, 2008 the FDA (2008) approved InPlex™ CF Molecular Test as an in vitro diagnostic device used to simultaneously detect and identify a panel of mutations and variants in the cystic fibrosis transmembrane conductance regulator (CFTR) gene in genomic DNA samples isolated from human peripheral whole blood specimens. The panel includes mutations and variants recommended by the 2004 American College of Medical Genetics (ACMG). The InPlex™ CF Molecular Test is a qualitative genotyping test that provides information intended to be used for cystic fibrosis carrier screening as recommended by ACMG and the 2005 American College of Obstetricians and Gynecologists (ACOG) for adults of reproductive age, as an aid in newborn screening for cystic fibrosis, and in confirmatory diagnostic testing for cystic fibrosis in newborns and children. The test is not indicated for use in fetal diagnostic or pre-implantation testing. This test is also not indicated for stand-alone diagnostic purposes and results should be used in conjunction with other available laboratory and clinical information.
On July 6, 2009 the FDA (FDA, 2009a) approved eSensor® CF Genotyping Test as an in vitro diagnostic device used to simultaneously detect and identify a panel of mutations and variants in the cystic fibrosis transmembrane conductance regulator (CFTR) gene in genomic DNA samples isolated from human peripheral whole blood specimens. The panel includes mutations and variants recommended by the 2004 American College of Medical Genetics (ACMG). The eSensor® CF Genotyping Test is a qualitative genotyping test that provides information intended to be used for cystic fibrosis carrier screening as recommended by ACMG and the 2005 American College of Obstetricians and Gynecologists (ACOG) for adults of reproductive age, as an aid in newborn screening for cystic fibrosis, and in confirmatory diagnostic testing for cystic fibrosis in newborns and children. The test is not indicated for use in fetal diagnostic or pre-implantation testing. This test is also not indicated for stand-alone diagnostic purposes and results should be used in conjunction with other available laboratory and clinical information.
On July 24, 2009 the FDA (FDA, 2009b) approved Verigene®CFTR and Verigene®CFTR PolyT Nucleic Acid Tests as qualitative in vitro diagnostic devices used to genotype a panel of mutations and variants in the cystic fibrosis transmembrane conductance regulator (CFTR) gene in genomic DNA isolated from human peripheral whole blood specimens. The panel includes mutations and variants recommended by the 2004 American College of Medical Genetics (ACMG) and the 2005 American College of Obstetricians and Gynecologists (ACOG). The Verigene®CFTR Nucleic Acid Test provides information intended to be used for carrier testing in adults of reproductive age and in confirmatory diagnostic testing of newborns and children. These tests are not indicated for use in fetal diagnostic or pre-implantation testing and not indicated for stand-alone diagnostic purposes and the results should be used in conjunction with other available laboratory and clinical information.
On December 11, 2009 the FDA (FDA, 2009c) approved e xTAG® Cystic Fibrosis 60 Kit v2 as a device used to simultaneously detect and identify a panel of mutations and variants in the cystic fibrosis transmembrane conductance regulator (CFTR) gene in human blood specimens. The panel includes mutations and variants currently recommended by the American College of Medical Genetics and American College of Obstetricians and Gynecologists (ACMG/ACOG), plus some of the world’s most common and North American prevalent mutations. The xTAG® Cystic Fibrosis 60 Kit v2 is a qualitative genotyping test which provides information intended to be used for carrier testing in adults of reproductive age, as an aid in newborn screening, and in confirmatory diagnostic testing in newborns and children. The kit is not indicated for use in fetal diagnostic or preimplantation testing. This kit is also not indicated for stand-alone diagnostic purposes. On December 15, 2016 a modification to this test was approved for new software thresholds for 2183/2184 variants.
On November 19, 2013 the FDA (2013b) approved Illumina MiSeqDx™ Cystic Fibrosis 139- Variant Assay is a qualitative in vitro diagnostic system used to simultaneously detect 139 clinically relevant cystic fibrosis disease‐causing mutations and variants of the cystic fibrosis transmembrane conductance regulator (CFTR) gene in genomic DNA isolated from human peripheral whole blood specimens. The variants include those recommended in 2004 by the American College of Medical Genetics (ACMG) and in 2011 by the American College of Obstetricians and Gynecologists (ACOG). The test is intended for carrier screening in adults of reproductive age, in confirmatory diagnostic testing of newborns and children, and as an initial test to aid in the diagnosis of individuals with suspected cystic fibrosis. The results of this test are intended to be interpreted by a board-certified clinical molecular geneticist or equivalent and should be used in conjunction with other available laboratory and clinical information. This test is not indicated for use for newborn screening, fetal diagnostic testing, preimplantation testing, or for stand‐alone diagnostic purposes.
On November 19, 2013 the FDA (2013a) also approved Illumina MiSeqDxTM Cystic Fibrosis Clinical Sequencing Assay as a targeted sequencing in vitro diagnostic system that re-sequences the protein coding regions and intron/exon boundaries of the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) gene in genomic DNA isolated from human peripheral whole blood specimens collected in K2EDTA. The test detects single nucleotide variants, and small InDels within the region sequenced, and additionally reports on two deep intronic mutations and two large deletions. The test is intended to be used on the Illumina MiSeqDx Instrument. The test is intended to be used as an aid in the diagnosis of individuals with suspected cystic fibrosis (CF). The test is most appropriate when the patient has an atypical or non-classic presentation of CF or when other mutation panels have failed to identify both causative mutations. The results of the test are intended to be interpreted by a board-certified clinical molecular geneticist or equivalent and should be used in conjunction with other available information including clinical symptoms, other diagnostic tests, and family history. This test is not indicated for use for stand-alone diagnostic purposes, fetal diagnostic testing, for pre-implantation testing, carrier screening, newborn screening, or population screening.
Guidelines and Recommendations
Practice Guidelines and Position Statements
Cystic Fibrosis Foundation
The Cystic Fibrosis Foundation (Farrell et al., 2017) convened a group of to develop clear and actionable consensus guidelines on the diagnosis of CF and to clarify diagnostic criteria and terminology for other disorders associated with CFTR mutations. The experts determined that “diagnoses associated with CFTR mutations in all individuals, from newborn to adult, be established by evaluation of CFTR function with a sweat chloride test. The latest mutation classifications annotated in the Clinical and Functional Translation of CFTR project (http://www.cftr2.org/index.php) should be used to aid in diagnosis.”
The committee approved 27 consensus statements:
- Sweat chloride testing should be performed according to approved procedural guidelines published in established, international protocols such as the CLSI 2009 Guidelines.
- Newborns with a positive CF newborn screen, to increase the likelihood of collecting an adequate sweat specimen, should have the test performed bilaterally and when the infant weighs >2 kg, and is at least 36 wk of corrected gestational age.
- Newborns greater than 36 wk gestation and >2 kg body weight with a positive CF newborn screen, or positive prenatal genetic test, should have sweat chloride testing performed as soon as possible after 10 d of age, ideally by the end of the neonatal period (4 wk of age).
- In infants with presumptive CF identified through NBS, CF treatment should not be delayed while efforts to establish a diagnosis of CF are initiated.
- Sweat chloride analysis should be performed within a few hours of sweat collection and the results and interpretations should be reported to clinicians and parents or patients, as soon as possible and certainly on the same day.
- In individuals presenting with a positive newborn screen, clinical features consistent with CF, or a positive family history, a diagnosis of CF can be made if the sweat chloride value is ≥60 mmol/L.
- Individuals who are screen-positive and meet sweat chloride criteria for CF diagnosis should undergo CFTR genetic testing if the CFTR genotype was not available through the screening process or is incomplete.
- In individuals with a positive newborn screen, a sweat chloride <30 mmol/L indicates that CF is unlikely.
- Individuals with clinical features that may be consistent with CF who have a sweat chloride <30 mmol/L indicates that CF is less likely. It may, however, be considered if evolving clinical criteria and/or CFTR genotyping support CF and not an alternative diagnosis.
- Individuals presenting with a positive newborn screen, symptoms of CF, or a positive family history, and sweat chloride values in the intermediate range (30-59 mmol/L) on two separate occasions may have CF. They should be considered for extended CFTR gene analysis and/or CFTR functional analysis.
- The latest classifications identified in the CFTR2 project (http://www.cftr2.org/index.php) should be used to aid with CF diagnosis:
- CF-causing mutation: individuals with 2 copies on separate alleles will likely have CF (clinical sweat confirmation needed)
- Mutation of varying clinical consequence (MVCC): a mutation that in combination with a CF-causing mutation or another MVCC mutation may result in CF
- Uncharacterized mutation/mutation of UNK: mutation that has not been evaluated by CFTR2 and may be disease causing or of variable clinical consequence or benign
- Non-CF-causing mutation: individuals with 1 or more are unlikely to have CF (as a result of that allele)
- In individuals presenting with a positive newborn screen, symptoms of CF, or a positive family history, the identification of 2 CF-causing mutations (defined by CFTR2) is consistent with a diagnosis of CF. Sweat chloride testing is necessary, though, to confirm the diagnosis.
- The absence of detection of 2 CF-causing CFTR mutations does not exclude a diagnosis of CF.
- If further CF functional testing is needed (NPD and ICM), it should be performed in a validated reference center with trained staff certified by the CF Foundation TDN or ECFS Clinical Trial Network.
- In individuals with a positive newborn screen but variable or uncharacterized CFTR mutations (<2 CF-causing mutations), the diagnosis of CF can be made by demonstrating CFTR dysfunction (a sweat chloride ≥ 60 mmol/L or CF-typical NPD or ICM).
- The term CRMS is used in the US for healthcare delivery purposes and CFSPID is used in other countries, but these both describe an inconclusive diagnosis following NBS.
- The term CRMS/CFSPID is reserved for individuals who screen positive without clinical features consistent with a diagnosis of CF.
- The definition of CRMS/CFSPID is an infant with a positive NBS test for CF and either:
- A sweat chloride value <30 mmol/L and 2 CFTR mutations, at least 1 of which has unclear phenotypic consequences OR
- An intermediate sweat chloride value (30-59 mmol/L) and 1 or 0 CF-causing mutations
- Children designated as CRMS/CFSPID should undergo at least one repeat sweat chloride test at CF centers with suitable expertise, such as an accredited CF center.
- Children designated as CRMS/CFSPID should have clinical evaluation performed by CF providers to identify the minority that may develop clinical symptoms.
- Children designated as CRMS/CFSPID can be considered for extended CFTR gene analysis (sequencing and or deletion duplication testing), as well as CFTR functional analysis (NPD/ICM) testing to further define their likelihood of developing CF.
- The decision to reclassify children designated as CRMS/CFSPID as CF is an integrated decision that should take into account functional assessment of CFTR (sweat chloride, and possibly NPD/ICM), CFTR genetic analysis, and clinical assessment by the CF clinicians caring for the patient.
- Genetic counseling should be offered to families of individuals followed for CRMS/CFSPID, including a discussion of the risk in future pregnancies.
- Research Recommendation: Infants with a designation of CRMS/CFSPID (by definition) do not have clinical features consistent with a diagnosis of CF and further research is needed to determine the prognosis and best practices for frequency and duration of follow-up.
- For individuals presenting with CF symptoms, the same diagnostic criteria recommended for the screened population for sweat chloride testing, CFTR genetic analysis, and CFTR functional testing should be used to confirm a CF diagnosis.
- The diagnosis of CFTR-related disorder has been defined as a monosymptomatic clinical entity (CBAVD/pancreatitis/bronchiectasis) associated with CFTR dysfunction that does not fulfill the diagnostic criteria for CF.
- Clinicians should avoid the use of terms like classic/nonclassic CF, typical/atypical CF, delayed CF, because these terms have no harmonized definition and could be confusing for families or caregivers.
The Cystic Fibrosis Foundation (Ren et al., 2018)also convened a multidisciplinary committee of CF caregivers to develop evidence based guidelines for CFTR modulator therapy. The committee defined patients with CF as individuals who met the above CFF criteria for diagnosis of CF, combined with evidence of abnormal CFTR function, as demonstrated by elevated sweat chloride, detection of two CF-causing CFTR mutations, or abnormal nasal potential differences.
For adults and children aged 6 years and older with CF due to gating mutations other than G551D or R117H, the guideline panel made a conditional recommendation for treatment with IVA. For those with the R117H mutation, the guideline panel made a conditional recommendation for treatment with IVA for 1) adults aged 18 years or older, and 2) children aged 6–17 years with a forced expiratory volume in 1 second (FEV1) less than 90% predicted. For those with the R117H mutation, the guideline panel made a conditional recommendation against treatment with IVA for 1) children aged 12–17 years with an FEV1 greater than 90% predicted, and 2) children less than 6 years of age. Among those with two copies of F508del, the guideline panel made a strong recommendation for treatment with IVA/LUM for adults and children aged 12 years and older with an FEV1 less than 90% predicted; and made a conditional recommendation for treatment with IVA/LUM for 1) adults and children aged 12 years or older with an FEV1 greater than 90% predicted, and 2) children aged 6–11 years.
American College of Obstetrics and Gynecology
The American College of Obstetrics and Gynecology (ACOG, 2017) recommends offering CF carrier screening to all women who are considering pregnancy or are currently pregnant. Expanded mutation panels which enhance the sensitivity for carrier screening can be considered for carrier detection, especially in non-Caucasian ethnic groups, but testing should not be repeated if performed previously (e.g. during previous pregnancy). If the patient is found to be a carrier, then her partner should be tested. They also indicate that newborn screening is not a replacement for carrier screening in a population.
Prenatal diagnosis is indicated after genetic counseling if both parents are carriers, or if the mother is a carrier and the father is unknown or unavailable for testing.
ACOG recommends that complete gene sequencing is not appropriate for use in carrier screening, rather reserved for patients with cystic fibrosis, patients with negative carrier screening but a family history of cystic fibrosis, males with congenital bilateral absence of the vas deferens, or newborns with a positive newborn screening after the standard 23 gene screen has a negative result.
They also recommend referral to genetic counseling for couples in which both partners are CF carriers, prenatal diagnosis and advanced reproductive technologies to decrease the risk of affected offspring should be discussed.
American College of Medical Genetics and Genomics
The American College of Medical Genetics and Genomics (ACMG) also recommends offering CF carrier screening to all women of reproductive age, regardless of ethnic background. Ideally, the testing would occur prior to pregnancy, but if the woman is pregnant, then she should be tested as early as possible during the pregnancy. ACMG also indicates that if the woman is found to be a CF carrier, then her reproductive partner should also be tested(Pletcher & Bocian, 2006). If the woman presents for testing late in the pregnancy, simultaneous testing of both the woman and the biologic father of the fetus should be considered. When there is a paternal family history of CF, carrier testing of the father is warranted.
Additionally, ACMG defines a panel of 23 mutations that includes the most common mutations found in a pan-ethnic population in the U.S. for use in routine CF carrier screening (ACMG, 2011; Watson et al., 2004). This 23-mutation panel incorporates all CF-causing mutations with a frequency of greater than or equal to 0.1% in the general U.S. population. ACOG also endorses the ACMG panel, and both organizations recommend against use of expanded mutation panels for routine CF carrier screening.
ACMG also recommends that testing for the IVS8 5T/7T/9T variant be performed only when carrier screening reveals a R117H mutation, or when a male is being evaluated for CBAVD, as R117H is causative of CF only if 5T is also present on the same chromosome, and 5T alone does not cause classic CF, but may cause CBAVD.
National Society of Genetic Counselors
The National Society of Genetic Counselors (NSGC) recommends that “Carrier testing for CF should be offered to all women of reproductive age, regardless of ancestry; preferably pre conceptionally. CF carrier testing should also be offered to any individual with a family history of CF and to partners of mutation carriers and people with CF.”
With regard to what mutations should be included in the carrier screening test, the NSGC states, “Carrier testing panels should include the mutations recommended by ACOG and ACMG. For individuals of non- Northern European descent, pan-ethnic panels that include additional mutations more commonly identified in minority populations are appropriate to consider. Focus general population CF screening practices on identifying carriers of established disease-causing CFTR mutations.”(Langfelder-Schwind et al., 2014)
The NSGC agrees with the ACMG regarding testing for IVS 8 5T/7T/9T as a reflex when mutation R117H is found in the CF carrier screen. They also assert that “in the absence of an R117H mutation, assessment of the intron 8 poly Tor TG tracts is not recommended for routine CF carrier testing.”
Billing/Coding/Physician Documentation Information
This policy may apply to the following codes. Inclusion of a code in this section does not guarantee that it will be reimbursed. For further information on reimbursement guidelines, please see Administrative Policies on the Blue Cross Blue Shield of North Carolina web site at www.bcbsnc.com. They are listed in the Category Search on the Medical Policy search page.
Applicable service codes: 81220, 81221, 81222, 81223, ,81224, 81412, 81479
| Code Number | PA Required | PA Not Required | Not Covered |
|---|---|---|---|
| 81220 | X | ||
| 81221 | X | ||
| 81222 | X | ||
| 81223 | X | ||
| 81224 | X | ||
| 81412 | X | ||
| 81479 | X |
Scientific Background and Reference Sources
ACMG. (2011). Technical Standards and Guidelines for CFTR Mutation Testing. STANDARDS AND GUIDELINES FOR CLINICAL GENETICS LABORATORIES.
ACOG. (2017). Committee Opinion No. 691: Carrier Screening for Genetic Conditions. Obstet Gynecol, 129(3), e41-e55. doi:10.1097/aog.0000000000001952
Baker, M. W., Atkins, A. E., Cordovado, S. K., Hendrix, M., Earley, M. C., & Farrell, P. M. (2016). Improving newborn screening for cystic fibrosis using next-generation sequencing technology: a technical feasibility study. Genet Med, 18(3), 231-238. doi:10.1038/gim.2014.209
Barrett, P. M., Alagely, A., & Topol, E. J. (2012). Cystic fibrosis in an era of genomically guided therapy. Hum Mol Genet, 21(R1), R66-71. doi:10.1093/hmg/dds345
Bell, S. C., De Boeck, K., & Amaral, M. D. (2015). New pharmacological approaches for cystic fibrosis: promises, progress, pitfalls. Pharmacol Ther, 145, 19-34. doi:10.1016/j.pharmthera.2014.06.005
Boucher, R. C. (2010). Bronchiectasis: a continuum of ion transport dysfunction or multiple hits? Am J Respir Crit Care Med, 181(10), 1017-1019. doi:10.1164/rccm.201002-0284ED
CF Foundation, U., Johns Hopkins University, The Hospital for Sick Children. (2017). The Clinical and Functional TRanslation of CFTR (CFTR2).
Clancy, J. P., & Jain, M. (2012). Personalized medicine in cystic fibrosis: dawning of a new era. Am J Respir Crit Care Med, 186(7), 593-597. doi:10.1164/rccm.201204-0785PP
Cohen-Cymberknoh, M., Shoseyov, D., & Kerem, E. (2011). Managing cystic fibrosis: strategies that increase life expectancy and improve quality of life. Am J Respir Crit Care Med, 183(11), 1463-1471. doi:10.1164/rccm.201009-1478CI
Elborn, J. S. (2016). Cystic fibrosis. Lancet. doi:10.1016/s0140-6736(16)00576-6
Farrell, P. M., Rosenstein, B. J., White, T. B., Accurso, F. J., Castellani, C., Cutting, G. R., . . . Campbell, P. W., 3rd. (2008). Guidelines for diagnosis of cystic fibrosis in newborns through older adults: Cystic Fibrosis Foundation consensus report. J Pediatr, 153(2), S4-s14. doi:10.1016/j.jpeds.2008.05.005
Farrell, P. M., White, T. B., Ren, C. L., Hempstead, S. E., Accurso, F., Derichs, N., . . . Sosnay, P. R. (2017). Diagnosis of Cystic Fibrosis: Consensus Guidelines from the Cystic Fibrosis Foundation. J Pediatr, 181s, S4-S15.e11. doi:10.1016/j.jpeds.2016.09.064
FDA. (2006a). Decision Summary ESENSOR CYSTIC FIBROSIS CARRIER DETECTION TEST 510(k) Premarket Notification.
FDA. (2006b). Decision Summary Tag It Cystic Fibrosis Carrier Detection System 510(k) Premarket Notification.
FDA. (2007). Decision Summary Cystic Fibrosis Genotyping Assay 510(k) Premarket Notification. U.S. Food and Drug Administration
FDA. (2008). Decision Summary Inplex CF Molecular Test 510(k) Premarket Notification. U.S. Food and Drug Administration
FDA. (2009a). Decision Summary eSensor® CF Genotyping Test 510(k) Premarket Notification. U.S. Food and Drug Administration
FDA. (2009b). Decision Summary Verigene® CFTR and Verigene® CFTR PolyT Nucleic Acid Tests 510(k) Premarket Notification. U.S. Food and Drug Administration
FDA. (2009c). Decision Summary xTAG® Cystic Fibrosis 60 Kit v2 510(k) Premarket Notification. U.S. Food and Drug Administration
FDA. (2013a). Decision Summary Illumina MiSeqDxTM Cystic Fibrosis Clinical Sequencing Assay 510(k) Premarket Notification. U.S. Food and Drug Administration
FDA. (2013b). Decision Summary Illumina MiSeqDx™ Cystic Fibrosis 139-Variant Assay 510(k) Premarket Notification. U.S. Food and Drug Administration
Grosse, S. D., Boyle, C. A., Botkin, J. R., Comeau, A. M., Kharrazi, M., Rosenfeld, M., & Wilfond, B. S. (2004). Newborn screening for cystic fibrosis: evaluation of benefits and risks and recommendations for state newborn screening programs. MMWR Recomm Rep, 53(Rr-13), 1-36.
Langfelder-Schwind, E., Karczeski, B., Strecker, M. N., Redman, J., Sugarman, E. A., Zaleski, C., . . . Darrah, R. (2014). Molecular testing for cystic fibrosis carrier status practice guidelines: recommendations of the National Society of Genetic Counselors. J Genet Couns, 23(1), 5-15. doi:10.1007/s10897-013-9636-9
Lim, R. M., Silver, A. J., Silver, M. J., Borroto, C., Spurrier, B., Petrossian, T. C., . . . Silver, L. M. (2016). Targeted mutation screening panels expose systematic population bias in detection of cystic fibrosis risk. Genet Med, 18(2), 174-179. doi:10.1038/gim.2015.52
Pletcher, B. A., & Bocian, M. (2006). Preconception and prenatal testing of biologic fathers for carrier status. American College of Medical Genetics. Genet Med, 8(2), 134-135. doi:10.109701.gim.0000200948.58427.e2
Pritchard, L. L. (2016). Respiratory Conditions Update: Cystic Fibrosis. FP Essent, 448, 35-43.
Ren, C. L., Morgan, R. L., Oermann, C., Resnick, H. E., Brady, C., Campbell, A., . . . Naureckas, E. T. (2018). Cystic Fibrosis Foundation Pulmonary Guidelines. Use of Cystic Fibrosis Transmembrane Conductance Regulator Modulator Therapy in Patients with Cystic Fibrosis. Ann Am Thorac Soc, 15(3), 271-280. doi:10.1513/AnnalsATS.201707-539OT
Schechter, M. S. (2014). Cystic fibrosis: An essential update. Contemporary Pediatrics.
Schrijver, I., Pique, L., Graham, S., Pearl, M., Cherry, A., & Kharrazi, M. (2016). The Spectrum of CFTR Variants in Nonwhite Cystic Fibrosis Patients: Implications for Molecular Diagnostic Testing. J Mol Diagn, 18(1), 39-50. doi:10.1016/j.jmoldx.2015.07.005
Simon, R. (2018). Cystic fibrosis: Overview of the treatment of lung disease-UpToDate. In A. Hoppin (Ed.), UpToDae.
Stafler, P., Mei-Zahav, M., Wilschanski, M., Mussaffi, H., Efrati, O., Lavie, M., . . . Blau, H. (2016). The impact of a national population carrier screening program on cystic fibrosis birth rate and age at diagnosis: Implications for newborn screening. J Cyst Fibros, 15(4), 460-466. doi:10.1016/j.jcf.2015.08.007
Straniero, L., Solda, G., Costantino, L., Seia, M., Melotti, P., Colombo, C., . . . Duga, S. (2016). Whole-gene CFTR sequencing combined with digital RT-PCR improves genetic diagnosis of cystic fibrosis. J Hum Genet. doi:10.1038/jhg.2016.101
Watson, M. S., Cutting, G. R., Desnick, R. J., Driscoll, D. A., Klinger, K., Mennuti, M., . . . Grody, W. W. (2004). Cystic fibrosis population carrier screening: 2004 revision of American College of Medical Genetics mutation panel. Genet Med, 6(5), 387-391. doi:10.109701.gim.0000139506.11694.7c
Wilschanski, M., Zielenski, J., Markiewicz, D., Tsui, L. C., Corey, M., Levison, H., & Durie, P. R. (1995). Correlation of sweat chloride concentration with classes of the cystic fibrosis transmembrane conductance regulator gene mutations. J Pediatr, 127(5), 705-710.
Policy Implementation/Update Information
1/1/2019 New policy developed. BCBSNC will provide coverage for genetic testing for cystic fibrosis when it is determined to be medically necessary because the criteria and guidelines are met. Medical Director review 1/1/2019. Policy noticed 1/1/2019 for effective date 4/1/2019. (jd)
Blue Cross and Blue Shield of North Carolina does not discriminate on the basis of race, color, national origin, sex, age or disability in its health programs and activities. Learn more about our non-discrimination policy and no-cost services available to you.
Information in other languages: Español 中文 Tiếng Việt 한국어 Français العَرَبِيَّة Hmoob ру́сский Tagalog ગુજરાતી ភាសាខ្មែរ Deutsch हिन्दी ລາວ 日本語
© 2026 Blue Cross and Blue Shield of North Carolina. ®, SM Marks of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield plans. All other marks and names are property of their respective owners. Blue Cross and Blue Shield of North Carolina is an independent licensee of the Blue Cross and Blue Shield Association.