As we referenced in our other recent provider news article about plan administration changes, effective January 1, 2026, Blue Cross and Blue Shield of North Carolina (Blue Cross NC) will become the plan administrator for Healthy Blue + Medicare℠ (HMO-POS D-SNP) serving eligible members across all 100 counties in North Carolina.
This transition includes:
- Claim submission
- Eligibility and benefit inquiries
- Authorization requests
- Remittance Inquiries / EOPs
- Claim status inquiries
Key dates and actions
- D-SNP member claims with dates of service before January 1, 2026, will continue to be submitted via the Elevance provider portal (Availity).
- D-SNP member claims with dates of service on or after January 1, 2026, should be submitted to Blue Cross NC EDI or Blue e Provider portals.
- Please notify your clearinghouse or trading partner to route D-SNP claims to Blue Cross NC, for dates of service on or after January 1, 2026
*Reminder: Blue Cross NC (CCFE) is the normal EDI HIPAA Submission channel, while Blue e is our provider portal for manual claims entry only.
Payor ID information
- Blue Cross NC does not require a Payor ID for claim submission. This differs from Elevance and submission through Availity. You or your clearing house / trading partner would use the normal Blue Cross NC "receiver" ID on all your electronic transmissions.
- Submit D-SNP claims for dates of service January 1, 2026, and beyond, as you would for any other Blue Cross NC member.
What’s not changing
- This change does not affect Medicaid claims. Continue submitting eligible services to Medicaid Direct.
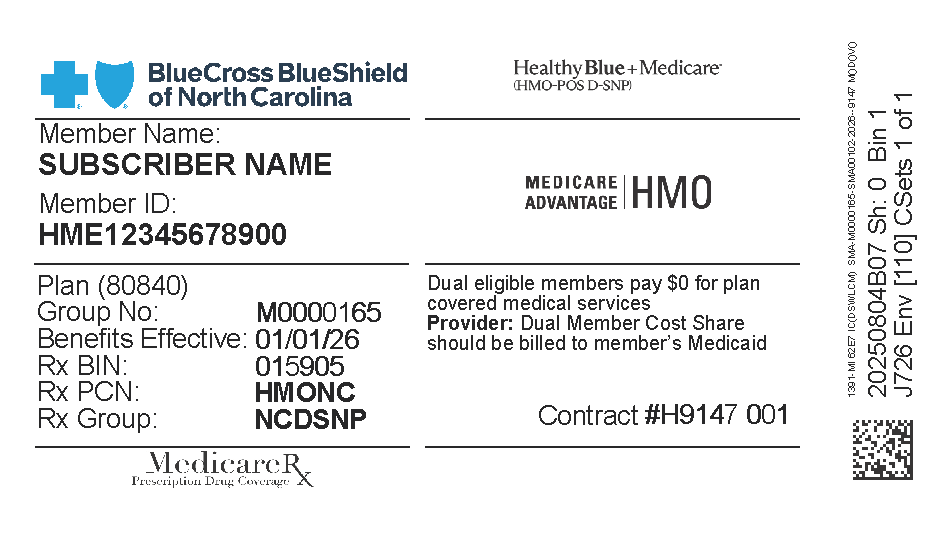
Member ID prefix guidance
- For members effective January 1, 2026, look for the “HME” prefix on their ID card. All transactions for these members should be directed to Blue Cross NC.
- For members with dates of service prior to January 1, 2026, and the L7H prefix, continue submitting transactions through Availity.
Member ID
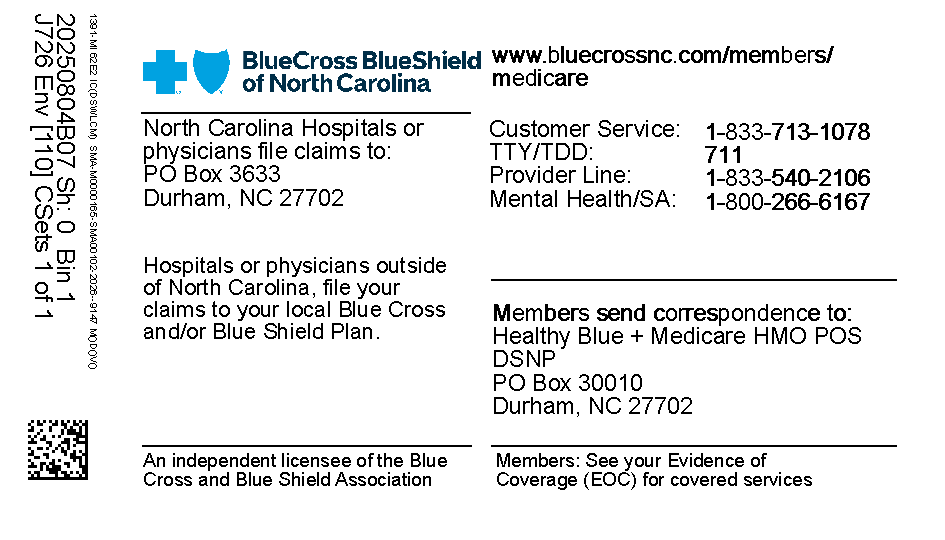
Members will receive a new member ID card with a new prefix. We have included an image of a sample card below:
Healthy Blue + Medicare (HMO-POS D-SNP) offers a zero-cost share plan with valuable extra benefits, making health care more accessible and affordable for eligible members. This transition allows Blue Cross NC to deliver more coordinated, efficient care and support for both providers and members.
If you have questions or need assistance, please contact provider services at 800-214-4484.
Blue Cross and Blue Shield of North Carolina does not discriminate on the basis of race, color, national origin, sex, age or disability in its health programs and activities. Learn more about our non-discrimination policy and no-cost services available to you.
Information in other languages: Español 中文 Tiếng Việt 한국어 Français العَرَبِيَّة Hmoob ру́сский Tagalog ગુજરાતી ភាសាខ្មែរ Deutsch हिन्दी ລາວ 日本語
© 2026 Blue Cross and Blue Shield of North Carolina. ®, SM Marks of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield plans. All other marks and names are property of their respective owners. Blue Cross and Blue Shield of North Carolina is an independent licensee of the Blue Cross and Blue Shield Association.