Effective January 1, 2026, Blue Cross and Blue Shield of North Carolina (Blue Cross NC) will become the plan administrator for Healthy Blue + Medicare℠ (HMO-POS D-SNP), serving eligible members across all 100 counties in North Carolina.
This transition marks the full insourcing of the existing Coordination Only Healthy Blue + Medicare (HMO-POS D-SNP), which Blue Cross NC currently offers in partnership with Elevance. Dual Special Needs Plans (D-SNPs) are specialized Medicare Advantage plans designed for individuals who are eligible for both Medicare and Medicaid.
Provider participation
- Providers will follow the existing credentialing, contracting, and enrollment process to participate in the D-SNP program.
- Providers currently participating in Medicare Advantage (MA) are already included in the D-SNP network.
- New providers interested in joining the MA network will follow the same process and be included in both MA and D-SNP.
Claims filing process
- Starting January 1, 2026, providers will file D-SNP claims using Blue Cross NC’s Blue e portal.
- Beginning January 1, 2026, providers can use Blue e not only for claims submission, but also for eligibility and benefits inquiries, authorization requests, remittance / Explanation of Payments (EOPs) inquiries, and claim status inquiries.
- For claims with dates of service prior to January 1, 2026, continue filing through the Elevance provider portal (Availity).
- If you use a clearinghouse, please notify them to route D-SNP claims to Blue Cross NC for dates of service on or after January 1, 2026.
- For more information on setting up both processes, please refer to the additional article on plan administration changes.
- This change does not affect Medicaid claims. Continue submitting eligible services to Medicaid Direct.
Network requirements
- In-network providers must adhere to standard Blue Cross NC requirements, including:
- Providers may not charge members, or balance bill, for any portion of a claim not covered by Medicare or Medicaid.
- Out-of-network providers must inform members prior to rendering services. Failure to do so may result in the provider being unable to bill the member.
These requirements remain unchanged with the insourcing of the D-SNP program.
Model of Care (MOC) training requirement
As part of Blue Cross NC’s D-SNP Model of Care, CMS requires all D-SNP-contracted and out-of-network providers who routinely see D-SNP members to complete:
- Initial and annual MOC training
- Attestation of completion
Failure to complete the required training may result in corrective action, including potential suspension or termination from the network.
Reimbursement policies
Effective January 1, 2026, Blue Cross NC Medicare reimbursement policies will apply to providers who serve members enrolled in Healthy Blue + Medicare (HMO-POS D-SNP). Our reimbursement policies are developed based on nationally accepted industry standards and coding principles. These policies may be superseded by mandates in provider, state, federal or CMS contracts and/or requirements. System logic or setup may prevent the loading of policies into the claims platforms in the same manner as described; however, Blue Cross NC strives to minimize these variations. To view the reimbursement policies, visit the provider self-service website.
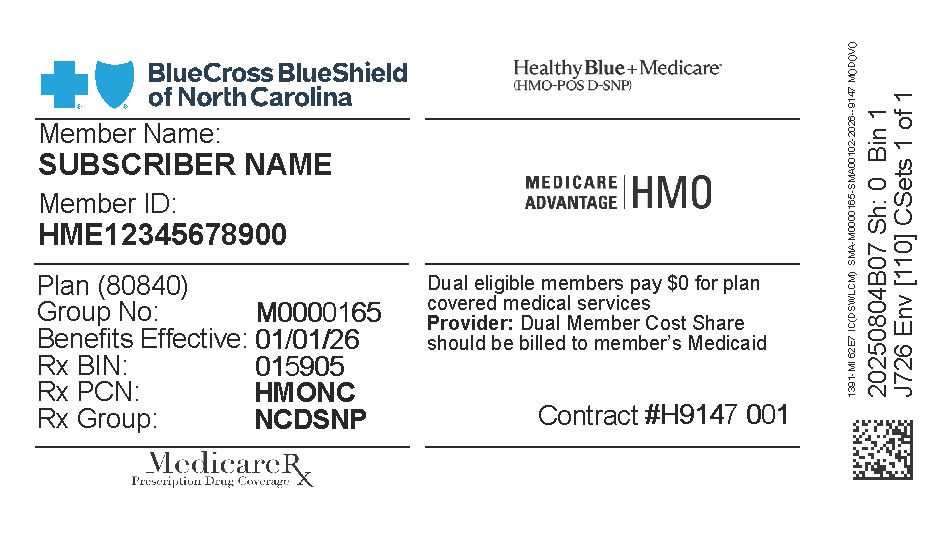
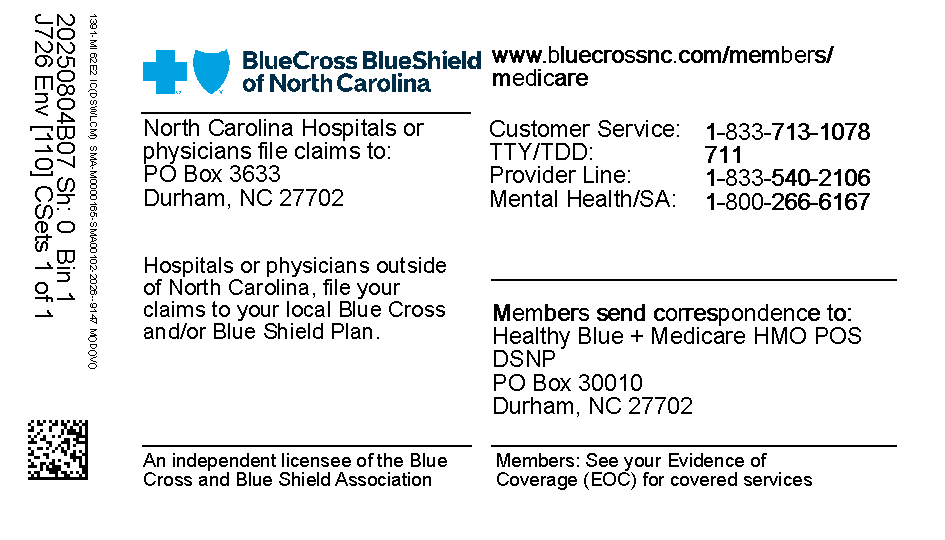
Member ID
Members will receive a new member ID card with a new prefix. We have included an image of a sample card below:
Interdisciplinary Care Team (ICT)
If you are a provider supporting a D-SNP enrollee’s Interdisciplinary Care Team (ICT), effective January 1, 2026, you will have access to view their Individualized Care Plan (ICP) in Care Affiliate via Blue e.
From the Home Screen in Care Affiliate:
- Enter the Member ID and Name, and tab out of the field
- Summary data on the member will display, including Care Plan data
- Select Care Plans
- Select D-SNP Case Management to be taken to the member’s ICP
- Within the ICP, you can navigate between Issues, Goals, and Interventions
If you need to contact a member of our D-SNP Case Management team regarding the ICP, you may call the Healthy Blue + Medicare Case Management department at 877-672-7647 OR send a secure email to DSNPMACaseManagement@bcbsnc.com. Our case management team is available Monday through Friday from 8 AM to 5 PM, so you can leave a detailed message after hours, and we will call or email you back.
Healthy Blue + Medicare (HMO-POS D-SNP) offers a zero-cost share plan with valuable extra benefits, making health care more accessible and affordable for eligible members. This transition allows Blue Cross NC to deliver more coordinated, efficient care and support for both providers and members.
If you have additional questions, or need assistance, please contact the Provider Service Line at 800-214-4484.
Blue Cross and Blue Shield of North Carolina does not discriminate on the basis of race, color, national origin, sex, age or disability in its health programs and activities. Learn more about our non-discrimination policy and no-cost services available to you.
Information in other languages: Español 中文 Tiếng Việt 한국어 Français العَرَبِيَّة Hmoob ру́сский Tagalog ગુજરાતી ភាសាខ្មែរ Deutsch हिन्दी ລາວ 日本語
© 2026 Blue Cross and Blue Shield of North Carolina. ®, SM Marks of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield plans. All other marks and names are property of their respective owners. Blue Cross and Blue Shield of North Carolina is an independent licensee of the Blue Cross and Blue Shield Association.